Ankylosingspondylitis (AS) has an incidence of approximately 0.1%–1.4%, and is a chronic inflammatory autoimmune disease characterized by ossification of the ligaments of the axial vertebral joints.1Some AS can progress to severe kyphotic deformity in the later stage, resulting in a sagittal imbalance of the spine and limited horizontal angle of view, affecting respiratory and digestive function, and seriously reducing the quality of life of patients.2,3During spinal joint ossification in AS, the thoracolumbar segment is most commonly affected, but the cervical and upper thoracic segments are also inevitably involved, and traditional physical therapy or orthopedic brace treatment is limited and surgical osteotomy correction is often required to improve the prognosis. Pedicle subtraction osteotomy (PSO) is widely used to correct AS kyphotic deformity in clinical practice, with positive clinical results.4Single-level vertebral column decancellation (VCD) was developed based on modified traditional vertebrectomy combined with the "eggshell technique."5Single-level VCD moves the osteotomy hinge point posteriorly to become an anterior open and posterior closed osteotomy, not only with a larger osteotomy angle than before but also with less bone removal.6However, no meta-analysis has been conducted to compare the safety and efficacy of VCD versus PSO in patients with thoracolumbar kyphotic deformity due to AS. This cohort study aimed to perform a meta-analysis to provide evidence-based medicine for selecting the appropriate surgical approach in clinical practice.
开云体育世界杯赔率
This meta-analysis followed the Cochrane handbook for conducting the study and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for reporting.7,8This study was registered with the PROSPERO database (http://www.crd.york.ac.uk/prospero/), and its registration no. is CRD42023408221. Two authors separately conducted literature retrieval, study eligibility, data extraction, and quality assessment, with inconsistencies resolved by discussion and decided by the corresponding author.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Literature Search
We conducted a computer search of PubMed, EMBASE, Web of Science, Cochrane Library, China National Knowledge Infrastructure (CNKI), Wan Fang Database, and Wei Pu Database to collect controlled clinical studies on the efficacy and safety of VCD and PSO for patients with AS with thoracolumbar kyphotic deformity. Our search covered the period from database establishment to March 2023. We restricted the language to English and Chinese. By keeping the literature that offered the most comprehensive information for overlapping patients, information duplication was avoided. The brief retrieval formula was "((ankylosing spondylitis) AND (kyphotic deformity)) AND ((vertebral column decancellation) OR (pedicle subtraction osteotomy))."
Inclusion and Exclusion Criteria
The inclusion criteria were as follows: 1) patients with thoracolumbar kyphotic deformity attributable to AS and treated by VCD or PSO at the lumbar or lower thoracic segments; and 2) the literature reported at least one of the following variables: operation time, intraoperative blood loss, Oswestry Disability Index (ODI) score, global kyphosis (GK), lumbar lordosis (LL), thoracic kyphosis (TK), the sagittal vertical axis (SVA), and complications.
Exclusion criteria were as follows: 1) patients were treated with more than 1 type of osteotomy; 2) missing data or mistakenly included literature; 3) patients had osteotomy at the cervical or the upper thoracic segments; 4) patients with AS had osteotomy due to another etiology, such as spinal tuberculosis or posttraumatic kyphosis; 5) review, meeting, expert opinion, case report, or literature for which we could not obtain the full text; and 6) animal experiments, in vitro/biomechanical studies.
Literature Screening and Data Extraction
两个独立调查人员筛选升ature according to the inclusion and exclusion criteria, then they extracted the data and cross-checked. In case of any disagreement, the issue was discussed and resolved. If necessary, the opinion of the third investigator was solicited, and the information was extracted using a predesigned data extraction form. The main information extracted from the data included the following: 1) general information of the included studies, consisting of the title, author, publication year, etc.; 2) study characteristics, including the study region, sample size, age, operation time, follow-up time, etc.; 3) outcome measures of interest, including intraoperative blood loss, ODI, GK, TK, LL, SVA, and complications; and 4) key elements of bias risk evaluation, including the selection of study population, comparability between groups, and measurement of exposure factors.
Literature Quality Evaluation
The evaluation of the included literature for risk of bias was independently completed by two evaluators and cross-checked. If there was disagreement on the results of the literature evaluation, the third party intervened to assist in the discussion and decision. The version 5.4 Bias Risk Assessment Tool recommended by the Cochrane Handbook was used to assess the quality of publications, including sequence generation, allocation concealment, blinding, data integrity, selective reporting and other potential biases, and the judgment of deviations was expressed as "low risk," "high risk," or "unclear risk." The Newcastle-Ottawa Scale risk bias assessment criteria were used to assess the quality of the cohort study literature, and articles with a total score of ≥ 7 were regarded as high-quality articles.
Statistical Analysis
Meta-analysis of the data from the included articles was performed using RevMan 5.4 software. Continuous variables were expressed as the mean difference (MD) and dichotomous variables as the odds ratio (OR), and the size of each pooled effect and its 95% confidence interval (CI) were calculated. Heterogeneity was analyzed using the chi-square test, and the size of heterogeneity was judged based on the I2value. When p > 0.1 or I2≤ 50%, heterogeneity between studies was not significant and the fixed-effect model was used for analysis; if p ≤ 0.1 or I2> 50%, heterogeneity between studies was significant and the random-effects model was used for analysis.
Results
Literature Screening Procedure and Studies Found
在这项研究中,497篇论文获得通过preliminary search, after which 175 repeated publications were eliminated by software. Titles and abstracts were then read, and 241 papers that obviously did not meet the inclusion criteria were eliminated. After careful reading of the full text and quality evaluation, 75 unqualified papers were further excluded, and 6 qualified papers6,9- - - - - -13were finally included. The paper screening process is presented inFig. 1. A total of 342 patients were included, consisting of 172 patients in the VCD group and 170 in the PSO group. The main characteristics of the included studies are presented inTable 1.

Flowchart illustrating the literature search and the selection of included studies. CNKI = China National Knowledge Infrastructure. Data added to the PRISMA template (from Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews.BMJ. 2021;372:n71) under the terms of the Creative Commons Attribution (CC BY 4.0) License (https://creativecommons.org/licenses/by/4.0/). Figure is available in color online only.
Basic characteristics of the included studies
| Authors & Year | Group | No. of Pts | Age (yrs) | No. (M/F) | Level (no.) | FU (mos) | Indication for Surgery |
|---|---|---|---|---|---|---|---|
| Wang et al., 20199 | VCD | 30 | 37.0±5.2 | 27/3 | L1 (2), L2 (16), L3 (12) | 29.8 ± 5.3 | Disturbed sagittal alignment |
| PSO | 27 | 40.3 ± 10.2 | 25/2 | L1 (3), L2 (15), L3 (9) | 27.9 ± 6.8 | ||
| Wang et al., 201910 | VCD | 36 | 38.1 ± 9.0 | 34/2 | L1 (5), L2 (19), L3 (12) | 28.8 ± 3.7 | Preop GK ranging from 40° to 120° |
| PSO | 25 | 38.5 ± 11.5 | 23/2 | L1 (4), L2 (14), L3 (7) | 30.2 ± 4.7 | ||
| Zhang et al., 20166 | VCD | 39 | 37.4 (28–54) | 26/13 | NR | NR | Disturbed sagittal alignment |
| PSO | 45 | 34.8 (23–47) | 31/14 | NR | NR | ||
| Qi et al., 201512 | VCD | 15 | 35.2 ± 8.9* | 31/2 | T12 (1), L2 (6), L3 (8) | NR | Disturbed sagittal alignment |
| PSO | 18 | L1, L3 (13); T12, L2 (4); T12, L3 (1) | NR | ||||
| Zhang et al., 202011 | VCD | 30 | 35.12 ± 8.26 | 17/13 | NR | NR | Disturbance of balance, inability to walk & stand upright |
| PSO | 30 | 35.01 ± 8.37 | 16/14 | NR | NR | ||
| Fan et al., 201913 | VCD | 22 | 36.3 ± 8.4 | 17/5 | NR | NR | GK >60° |
| PSO | 25 | 36.8 ± 8.2 | 19/6 | NR | NR |
FU = follow-up; NR = not reported; pts = patients.
Represents overall mean age of the 33 patients in the study.
Quality Analysis of Included Studies
Risk assessment for the 6 cohort studies included in the analysis was conducted using the Cochrane Bias Risk Assessment Tool and is presented inFig. 2. The quality of nonrandomized controlled trials was assessed using the Newcastle-Ottawa Scale. All included studies scored between 6 and 9 points, indicating high quality.Table 2provides a summary of the quality scores for each study.

Risk of bias graph for each included study. Figure is available in color online only.
Quality assessment using the Newcastle-Ottawa Scale for each nonrandomized controlled trial
| Variable | Wang et al., 20199 | Wang et al., 201910 | Zhang et al., 20166 | Qi et al., 201512 | Zhang et al., 202011 | Fan et al., 201913 |
|---|---|---|---|---|---|---|
| Selection | ||||||
| Representativeness of exposed cohort | 1 | 1 | 1 | 1 | 1 | 1 |
| Selection of nonexposed cohort | 1 | 1 | 1 | 1 | 1 | 1 |
| Ascertainment of exposure | 1 | 1 | 1 | 1 | 1 | 1 |
| Demonstration that outcome of interest was not present at start of study | 1 | 1 | ||||
| Comparability | ||||||
| Study controlled for age or sex | 1 | 1 | 1 | 1 | 1 | 1 |
| Study controlled for any additional factor | 1 | 1 | 1 | |||
| Outcome | ||||||
| Assessment of outcome | 1 | 1 | 1 | 1 | 1 | 1 |
| FU long enough for outcomes to occur | 1 | 1 | 1 | 1 | 1 | 1 |
| Adequacy of FU of cohort | 1 | 1 | 1 | 1 | 1 | 1 |
| Total | 9 | 8 | 8 | 8 | 7 | 7 |
Meta-Analysis Findings
Operation Time
A total of 5 studies used operation time as an outcome measure, with 136 patients in the VCD group and 145 in the PSO group. The heterogeneity test (p < 0.00001, I2= 97%)认为有重要的异性geneity between the studies, and a meta-analysis was performed using a random-effects model. The results showed the following: MD −80.28, 95% CI −150.07 to −10.48), p = 0.02 (Fig. 3), which suggested that the application of VCD in the correction of AS with thoracolumbar kyphosis can shorten the operation time compared with PSO, and that the difference was statistically significant.

Forest plot of operation time. Figure is available in color online only.
Intraoperative Blood Loss
Intraoperative blood loss was counted in 6 studies, with 172 patients in the VCD group and 170 in the PSO group. The heterogeneity test (p < 0.00001, I2= 91%) suggested that there was significant heterogeneity between the studies, and a meta-analysis was performed using a random-effects model. The results showed that intraoperative blood loss in the VCD group was significantly lower than that in the PSO group (MD −274.92, 95% CI −506.63 to −43.20, p = 0.02) (Fig. 4),表明VCD手术方法了definite effect on the reduction of intraoperative blood loss in patients.

Forest plot of intraoperative blood loss. Figure is available in color online only.
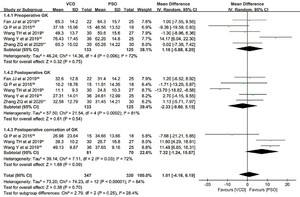
Oswestry Disability Index
Preoperative ODI score was reported in 3 papers, and heterogeneity test results showed p = 0.49; I2= 0%. Meta-analysis was performed using a fixed-effect model, and the results showed that there was no significant difference in the preoperative ODI scores between the VCD and PSO group (MD 1.14, 95% CI −1.88 to 4.16, p = 0.46).
Postoperative ODI was reported in 3 papers, and heterogeneity test results showed p = 0.46; I2= 0%. Meta-analysis was performed using a fixed-effect model, and the results showed that there was no significant difference in postoperative ODI scores between the VCD and PSO group (MD 0.26, 95% CI −0.47 to 0.98, p = 0.49) (Fig. 5,Supplementary Fig. 1).

Forest plot of ODI. Figure is available in color online only.
Global Kyphosis
Preoperative GK was reported in 5 papers, and heterogeneity test results showed p = 0.006; I2= 72%. Meta-analysis was performed using a random-effects model, and the results showed that there was no significant difference in preoperative GK between the VCD and PSO group (MD 1.16, 95% CI –5.88 to 8.20, p = 0.75).
Postoperative GK was reported in 5 papers, and heterogeneity test results showed p = 0.0002; I2= 81%. Meta-analysis was performed using a random-effects model, and the results showed that there was no significant difference in postoperative GK between the VCD and PSO group (MD −2.33, 95% CI −9.80 to 5.15, p = 0.54).
Postoperative correction of GK was reported in 3 papers, and heterogeneity test results showed p = 0.03; I2= 72%. Meta-analysis was performed using a random-effects model, and the results showed that there was no significant difference in postoperative correction of GK between the VCD and PSO group (MD 7.32, 95% CI −1.24 to 15.87, p = 0.09) (Fig. 6).

Forest plot of GK. Figure is available in color online only.
Thoracic Kyphosis
Preoperative TK was reported in 4 papers, and heterogeneity test results showed p = 0.15; I2= 43%. Meta-analysis was performed using a fixed-effect model, and the results showed that there was no significant difference in preoperative TK between the VCD and PSO group (MD −2.52, 95% CI −6.53 to 1.49, p = 0.22).
Postoperative TK was reported in 4 papers, and heterogeneity test results showed p = 0.22; I2= 33%. Meta-analysis was performed using a fixed-effect model, and the results showed that there was no significant difference in postoperative TK between the VCD and PSO group (MD −0.43, 95% CI −4.71 to 3.85, p = 0.84).
Postoperative correction of TK was reported in 2 papers, and heterogeneity test results showed p = 0.03; I2= 79%. Meta-analysis was performed using a random-effects model, and the results showed that there was no significant difference in postoperative correction of TK between the VCD and PSO group (MD −0.51, 95% CI −2.61 to 1.58, p = 0.63) (Supplementary Figs. 2and3).
Lumbar Lordosis
Preoperative LL was reported in 5 papers, and heterogeneity test results showed p = 0.83; I2= 0%. Meta-analysis was performed using a fixed-effect model, and the results showed that there was no significant difference in preoperative LL between the VCD and PSO group (MD 2.55, 95% CI −0.81 to 5.90, p = 0.14).
Postoperative LL was reported in 5 papers, and heterogeneity test results showed p = 0.001; I2= 77%. Meta-analysis was performed using a random-effects model, and the results showed that there was no significant difference in postoperative LL between the VCD and PSO group (MD −4.55, 95% CI −12.24 to 3.14, p = 0.25).
Postoperative correction of LL was reported in 3 papers, and heterogeneity test results showed p = 0.001; I2= 85%. Meta-analysis was performed using a random-effects model, and the results showed that there was no significant difference in postoperative correction of LL between the VCD and PSO group (MD 12.42, 95% CI −2.98 to 27.82, p = 0.11) (Supplementary Fig. 4).
Sagittal Vertical Axis
Preoperative SVA was counted in 3 studies, with 81 patients in the VCD group and 70 in the PSO group. The heterogeneity test (p = 0.90, I2= 0%)认为有重大heterogeneity between the studies, and a meta-analysis was performed using a fixed-effect model, and the results showed that there was no significant difference in preoperative SVA between the VCD and PSO group (MD 1.58, 95% CI −1.98 to 5.13, p = 0.38).
Postoperative SVA was counted in 3 studies, with 81 patients in the VCD group and 70 in the PSO group. The heterogeneity test (p < 0.0001, I2= 91%) suggested that there was significant heterogeneity between the studies, and a meta-analysis was performed using a fixed-effect model, and the results showed that postoperative SVA in the VCD group was significantly lower than that in the PSO group (MD −36.58, 95% CI −38.31 to −34.85, p < 0.00001), which indicates that the VCD surgical approach had a positive effect in improving sagittal imbalance of the spine in patients.
Postoperative correction of the SVA was counted in 4 studies, with 120 patients in the VCD group and 115 in the PSO group. The heterogeneity test (p = 0.76, I2= 0%)认为有重大heterogeneity between the studies, and a meta-analysis was performed using a fixed-effect model, and the results showed that there was no significant difference in postoperative correction of the SVA between the VCD and PSO group (MD 3.91, 95% CI −7.46 to 15.29, p = 0.50) (Supplementary Figs. 5and6).
Complications
Total complications were reported in 4 papers, and heterogeneity test results showed p = 0.86; I2= 0%. Meta-analysis was performed using a fixed-effect model, and the results showed that there was no significant difference in total complications between the VCD and PSO group (MD 1.05, 95% CI 0.57 to 1.94, p = 0.87). Dural tears were reported in 3 papers, and heterogeneity test results showed p = 0.94; I2= 0%. Meta-analysis was performed using a fixed-effect model, and the results showed that there was no significant difference in dural tears between the VCD and PSO group (MD 1.06, 95% CI 0.41 to 2.75, p = 0.91). Deep wound infection was reported in 3 papers, and heterogeneity test results showed p = 0.93; I2= 0%. Meta-analysis was performed using a fixed-effect model, and the results showed that there was no significant difference in deep wound infection between the VCD and PSO group (MD 0.52, 95% CI 0.09 to 2.95, p = 0.46). Sagittal translation at the osteotomy site was reported in 3 papers, and heterogeneity test results showed p = 0.74; I2= 0%. Meta-analysis was performed using a fixed-effect model, and the results showed that there was no significant difference in sagittal translation at the osteotomy site between the VCD and PSO group (MD 1.04, 95% CI 0.39 to 2.77, p = 0.93). Neurological deficit was reported in 3 papers, and heterogeneity test results showed p = 0.45; I2= 0%. Meta-analysis was performed using a fixed-effect model, and the results showed that there was no significant difference in neurological deficit between the VCD and PSO group (MD 1.49, 95% CI 0.20 to 11.18, p = 0.70) (Supplementary Figs. 7and8).
Heterogeneity and Sensitivity Analysis
分析显示高异质性的值for intraoperative blood loss and operation time. To assess the impact of heterogeneity on the results, a sensitivity analysis was conducted by removing individual studies from the analysis of operation time. The findings remained consistent with the original conclusions, suggesting that heterogeneity had minimal influence on the study outcomes. The heterogeneity observed in the analysis may be attributed to variations in operator skill levels. Specifically, the exclusion of Zhang et al.6reduced heterogeneity in intraoperative blood loss by 20%, whereas removal of other studies did not result in significant changes. Factors contributing to heterogeneity may include differences in surgeon experience, operating techniques, methods for measuring intraoperative blood loss, and completeness and accuracy of case records.
Publication Bias
The study included 6 articles and tested all outcome measures for publication bias. The funnel plot was visually assessed for each outcome measure, and it appeared to be mostly symmetrical, indicating a low likelihood of publication bias.Supplementary Figs. 9- - - - - -16provide supporting evidence for this finding.
Discussion
Patients with AS gradually form ankylosing kyphotic deformity due to long-term inflammatory activity leading to vertebral osteophyte hyperplasia and ligament ossification.14,15Kyphosis leads to the pathological forward movement of the trunk center of gravity. In order to restore the low-energy–expenditure position and reduce the energy expenditure of the body, patients usually need compensatory hip extension and knee flexion. Through the retroversion of the pelvis, the trunk center of gravity is repositioned on the neutral position line. However, when the kyphotic deformity cannot maintain balance through compensation, the patient’s mobility is significantly limited and the quality of life is dramatically reduced.16,17In recent years, the quality of life of patients with AS kyphotic deformity has been further improved by surgical osteotomy and correction to restore spinal sequence, reconstruct sagittal balance, and improve the maxillo-brow angle.18Commonly used osteotomy classification methods in clinical practice mainly include the following: opening wedge osteotomy, closing wedge osteotomy, and closing–opening wedge osteotomy.19- - - - - -23
The main mode of closing wedge osteotomy is PSO, which uses the posterior wall of the vertebral body as the wedge base, resects the lamina, pedicle, and transverse process through a posterior wedge to the anterior cortex of the vertebral body, and uses the anterior cortical bone as the center of the rotational hinge to close the wedge space of the anterior and middle columns. The degree of PSO correction increases with the height of the osteotomy, and vertebral body height and anteroposterior diameter are geometrical constraints on the orthopedic effect of PSO. Because of the limitation of the PSO angle, a 2-level PSO is usually required to reconstruct sagittal balance for severe AS kyphotic deformity.24Although studies have demonstrated that 1-stage, 2-level osteotomy is safe and effective, additional osteotomy procedures inevitably increase operative time, intraoperative blood loss, and surgery-related complications.25Wang and Lenke5combined VCR with the PSO technique and modified it to form the VCD technique. The advantage of VCD is that it effectively increases the osteotomy angle while reducing the osteotomy amount. Compared with the traditional anterior open and posterior closed osteotomy, VCD not only effectively removes the cancellous bone, but also preserves part of the cancellous bone as the "bone cage" on this basis. The positive value of this move lies in the fact that the built-in amount of artificial support is reduced, which not only improves the safety of spinal osteotomy, but also avoids the adverse effects caused by excessive shortening of the spine during orthopedic surgery, which not only achieves the surgical goal but also significantly improves the surgical safety.
The results of our meta-analysis showed that VCD could save operation time and reduce intraoperative blood loss compared with PSO. Previous studies have shown that PSO requires a longer operation time in cases of AS with thoracolumbar kyphotic deformity, because PSO is a 3-column osteotomy of the vertebral body that relies on collapse and closure of the osteotomized vertebral body to later correct the kyphotic deformity, and the deep osteotomy is often performed during the closure process.9Among the literature included in this meta-analysis, Zhang et al.11found that the operation time of 258.6 ± 49.2 minutes in the single-level VCD group was significantly shorter than the time of 396 ± 73.8 minutes in the 2-level PSO group, and that the intraoperative blood loss of 985.62 ± 65.17 ml was significantly lower than the blood loss of 1353.28 ± 65.28 ml in the 2-level PSO group. However, in terms of the operation time, the heterogeneity of this study was high. Meta-analysis was performed again after removing the published studies one by one. After combining the results, the difference in the outcome measures was statistically significant.
非均质性的主要原因可能是由于differences in surgeon experience and operating habits, differences in surgical instruments used, proficiency in surgical techniques, and differences in the way surgical time is recorded. In addition, the learning curve can affect the results to some extent. Therefore, for patients with severe AS and thoracolumbar kyphosis, the use of PSO is bound to increase the osteotomy level, thereby prolonging the operation time and thus leading to increased intraoperative blood loss. When VCD osteotomy is used, the anterior side is relatively opened while shortening the posterior side, avoiding the risk of nerve injury caused by excessive compression of the convex side and vascular damage caused by the excessive opening of the concave side. At the same time, the preserved partial cancellous bone is conducive to the fusion and stability of the bone, so the single-level osteotomy can obtain a relatively safer and more effective orthopedic effect, and the shortening of the operation time greatly reduces intraoperative blood loss.
GK, TK, and LL are important parameters for judging the sagittal balance of the spine in clinical practice. Comparing the changes in parameter values before and after treatment can determine the surgical treatment effect on patients. In this meta-analysis, the corresponding indicators after treatment were compared between the two groups. The results showed that there was no significant difference in GK, TK, and LL (p > 0.05). This suggests that VCD is similar to PSO in correcting AS kyphotic deformity in terms of remodeling spinal alignment. In addition, the ODI score in both groups was significantly improved compared with that before treatment. There was no significant difference in postoperative ODI between the two groups (p > 0.05), indicating that the prognosis of the two groups was similar.
Most PSOs reported in the literature are generally performed in the apical lumbar lordosis region (L2 or L3), and single-level PSOs can achieve an average of 30°–40° correction.23,26Xu et al.27compared the data of patients with AS kyphotic deformity treated with single-level PSO and 2-level PSO, and pointed out that 2-level PSO had a better orthopedic effect for patients with severe thoracolumbar kyphosis and LL loss. These authors also noted that although operation time and intraoperative blood loss were greater for 2-level osteotomy than for single-level osteotomy, there was no significant difference in the incidence rate of complications between the two groups. Unlike PSO, posterior column resection in VCD resembles closing wedge osteotomy, but the apex of its wedge moves posteriorly to the midpoint of the sagittal view of the vertebral body. With this apex as the center of the rotating hinge, starting from this point, the anterior column of the vertebral body is opened and shortened by cutting anteriorly parallel along the endplate or directly closing the posterior column and opening the anterior column. Wang et al.9相比30和患者之间的校正erwent single-level VCD and 27 patients who underwent single-level PSO, in which the mean correction was 50.8° ± 9.7° in the VCD group, 38.5° ± 6.1° in the PSO group, 174.8 ± 64.9 mm in the VCD group, and 159.2 ± 97.1 mm in the PSO group, and VCD was superior to PSO in terms of correction and sagittal reconstruction compared with PSO. Wang et al.10also compared AS correction between single-level VCD and PSO, with 49.13° ± 9.87° GK correction in the VCD group and 37.65° ± 9.16° in the PSO group. In addition, the analysis of surgery-related and postoperative complications in this study showed that there was no statistical difference in the incidence rate of complications between the two groups.
This study also has shortcomings, as follows: 1) none of the studies included were randomized controlled trials—only 6 comparative studies were found, all of which were retrospective, and confounding factors and potential selection bias existed; 2) it is not possible to fully understand the details of the conduct of each study, such as the physician’s proficiency with the VCD or PSO method and the authenticity and completeness of the case data; and 3) most publications in this study include small samples, which will have a definite impact on the reliability of the results and will require more large-sample multicenter randomized controlled trials to verify the conclusions.
Conclusions
Based on the current meta-analysis results, the clinical effect of VCD and PSO in the correction of AS kyphotic deformity was similar, and the reconstruction of sagittal balance and improvement of quality of life were satisfactory in both procedures, but the former had shorter operation time, less intraoperative blood loss, better sagittal reconstruction effect, and a larger range of single-level osteotomy angles. When conditions allowed, single-level VCD was recommended to correct AS kyphotic deformity.
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author Contributions
Conception and design: Luan. Acquisition of data: Luan, Peng. Analysis and interpretation of data: Luan, Peng. Drafting the article: Luan, Liu. Critically revising the article: all authors. Reviewed submitted version of manuscript: all authors. Approved the final version of the manuscript on behalf of all authors: Song. Statistical analysis: Song, Luan, Liu. Administrative/technical/material support: Song. Study supervision: Song.
Supplemental Information
Online-Only Content
Supplemental material is available with the online version of the article.
Supplementary Figs. 1–16.//www.prize-show.com/doi/suppl/10.3171/2023.4.SPINE23329.
Data Availability
The data sets generated and analyzed during the current study are not publicly available due to restrictions on ethical approvals involving patient data and anonymity, but may be requested from the corresponding author.
Systematic review registration no.: CRD42023408221 (www.crd.york.ac.uk/prospero/)
References
-
1 ↑
DakwarE,ReddyJ,ValeFL,UribeJS.A review of the pathogenesis of ankylosing spondylitis.Neurosurg Focus.2008;24(1):E2.
-
3 ↑
KimKT,ParkDH,LeeSH,LeeJH.Results of corrective osteotomy and treatment strategy for ankylosing spondylitis with kyphotic deformity.Clin Orthop Surg.2015;7(3):330- - - - - -336.
-
4 ↑
LuanH,LiuK,KahaerA,et al.Pedicle subtraction osteotomy for the corrective surgery of ankylosing spondylitis with thoracolumbar kyphosis: experience with 38 patients.BMC Musculoskelet Disord.2022;23(1):731.
-
5 ↑
WangY,LenkeLG.Vertebral column decancellation for the management of sharp angular spinal deformity.Eur Spine J.2011;20(10):1703- - - - - -1710.
-
6 ↑
ZhangX,ZhangZ,WangJ,et al.Vertebral column decancellation: a new spinal osteotomy technique for correcting rigid thoracolumbar kyphosis in patients with ankylosing spondylitis.Bone Joint J.2016;98-B(5):672-678.
-
7 ↑
MoherD,LiberatiA,TetzlaffJ,AltmanDG.Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement.Int J Surg.2010;8(5):336- - - - - -341.
-
8 ↑
PhanK,MobbsRJ.Systematic reviews and meta-analyses in spine surgery, neurosurgery and orthopedics: guidelines for the surgeon scientist.J Spine Surg.2015;1(1):19- - - - - -27.
-
9 ↑
WangT,ZhengG,WangY,ZhangX,HuF,WangY.Comparison of 2 surgeries in correction of severe kyphotic deformity caused by ankylosing spondylitis: vertebral column decancellation and pedicle subtraction osteotomy.World Neurosurg.2019;127:e972- - - - - -e978.
-
10 ↑
WangY,XueC,SongK,et al.Comparison of loss of correction between PSO and VCD technique in treating thoracolumbar kyphosis secondary to ankylosing spondylitis, a minimum 2 years follow-up.J Orthop Surg Res.2019;14(1):137.
-
11 ↑
ZhangZ,KongZ,ZhangF,LiuX.Comparison of the efficacy of single-segment spine decancellous osteotomy and double-segment transpedicular osteotomy to correct ankylosing spondylitis and kyphosis.Zhongwai Yiliao.2020;39(26):64-66,72.
-
12 ↑
QiP,SongK,ZhangY,WangY,CuiG.Comparison of the clinical effect in ankylosing spondylitis-related kyphosis between one-level vertebral column decancellation and two-level pedicle subtraction osteotomy.Zhongguo Jizhu Jisui Zazhi.2015;25(9):775- - - - - -780.
-
13 ↑
FanJ,LiY,JinZ,et al.A comparative study on clinical effect between single-segment spine cancellous osteotomy and double-segment transpedicular osteotomy in correction of kyphosis in patients with ankylosing spondylitis.Linchuang Shiyan Yixue Zazhi.2019;18(23):2557- - - - - -2560.
-
14 ↑
XiongY,CaiM,XuY,et al.Joint together: the etiology and pathogenesis of ankylosing spondylitis.Front Immunol.2022;13:996103.
-
15 ↑
LiuC,HuF,HuW,et al.Clinical results of utilizing the satellite rod technique in treating ankylosing spondylitis kyphosis.Orthop Surg.2022;14(9):2180- - - - - -2187.
-
16 ↑
ShinJK,LeeJS,GohTS,SonSM.Correlation between clinical outcome and spinopelvic parameters in ankylosing spondylitis.Eur Spine J.2014;23(1):242- - - - - -247.
-
17 ↑
SongK,ZhengG,ZhangY,ZhangX,MaoK,WangY.A new method for calculating the exact angle required for spinal osteotomy.Spine (Phila Pa 1976).2013;38(10):E616- - - - - -E620.
-
18 ↑
TominagaR,FukumaS,YamazakiS,et al.Relationship between kyphotic posture and falls in community-dwelling men and women: the Locomotive Syndrome and Health Outcome in Aizu Cohort Study.Spine (Phila Pa 1976).2016;41(15):1232- - - - - -1238.
-
19 ↑
ChangKW,ChenHC,ChenYY,LinCC,HsuHL,CaiYH.Sagittal translation in opening wedge osteotomy for the correction of thoracolumbar kyphotic deformity in ankylosing spondylitis.Spine (Phila Pa 1976).2006;31(10):1137- - - - - -1142.
-
20
ChangKW,ChengCW,ChenHC,ChangKI,ChenTC.Closing-opening wedge osteotomy for the treatment of sagittal imbalance.Spine (Phila Pa 1976).2008;33(13):1470- - - - - -1477.
-
21
BerjanoP,AebiM.Pedicle subtraction osteotomies (PSO) in the lumbar spine for sagittal deformities.Eur Spine J.2015;24(suppl 1):S49- - - - - -S57.
-
22
KollerH,KollerJ,MayerM,HempfingA,HitzlW.Osteotomies in ankylosing spondylitis: where, how many, and how much?.Eur Spine J.2018;27(1 suppl 1):70- - - - - -100.
-
23 ↑
QianBP,WangXH,QiuY,et al.The influence of closing-opening wedge osteotomy on sagittal balance in thoracolumbar kyphosis secondary to ankylosing spondylitis: a comparison with closing wedge osteotomy.Spine (Phila Pa 1976).2012;37(16):1415- - - - - -1423.
-
24 ↑
ChenIH,ChienJT,YuTC.Transpedicular wedge osteotomy for correction of thoracolumbar kyphosis in ankylosing spondylitis: experience with 78 patients.Spine (Phila Pa 1976).2001;26(16):E354- - - - - -E360.
-
25 ↑
ZhengGQ,SongK,ZhangYG,et al.Two-level spinal osteotomy for severe thoracolumbar kyphosis in ankylosing spondylitis. Experience with 48 patients.Spine (Phila Pa 1976).2014;39(13):1055- - - - - -1058.
-
26 ↑
ZhangPC,DengQ,ShengWB,et al.The sagittal parameters and efficacy of pedicle subtraction osteotomy in patients with ankylosing spondylitis and kyphosis under different lumbar sagittal morphologies.Int J Gen Med.2021;14:361- - - - - -370.
-
27 ↑
XuH,ZhangY,ZhaoY,ZhangX,XiaoS,WangY.Radiologic and clinical outcomes comparison between single- and two-level pedicle subtraction osteotomies in correcting ankylosing spondylitis kyphosis.Spine J.2015;15(2):290- - - - - -297.