Inrecent years, reperfusion therapies such as endovascular thrombectomy (EVT) and intravenous thrombolysis have been shown to be effective treatments for acute ischemic stroke (AIS).1–3Endovascular therapy has become increasingly recognized as the standard approach for strokes induced by large-vessel occlusion (LVO), particularly in the anterior circulation.4Despite a successful EVT recanalization rate of up to 90%, favorable outcomes have been achieved in only about 47% of patients as reported in randomized controlled trials, and this number may be even lower in real-world settings.5
Previous studies have shown that reocclusion, which occurs in approximately 10% of patients,6–8may be a significant cause of poor prognosis due to endothelial damage or platelet aggregation caused by severe atherosclerotic stenosis. To address reocclusion, antiplatelet drugs such as glycoprotein IIb/IIIa receptor antagonists, including tirofiban, eptifibatide, and abciximab, have been applied because of their short half-life, rapid action, and reversible effect on platelet aggregation.9–13Given its effectiveness in acute coronary syndromes, tirofiban is the most commonly used antagonist in clinical practice despite limited evidence. Most studies on the role of tirofiban in the endovascular treatment of AIS have been observational, retrospective, and small-sample or single-center, and have produced conflicting findings.13–17Recently, the RESCUE BT trial, a high-quality, randomized, placebo-controlled study, was published inJAMA.13Unfortunately, this study did not provide positive evidence supporting the use of intravenous tirofiban before EVT for AIS.13
The objective of this study was to assess the effectiveness and safety of tirofiban in improving functional outcomes of direct thrombectomy for acute anterior circulation occlusion. Additionally, we sought to identify the specific patient population that may benefit from tirofiban treatment.
开云体育世界杯赔率
Data Collection and Processing
The ethics committee of Nanjing Drum Tower Hospital approved this study. Retrospective data on patients with AIS who underwent EVT between January 2020 and December 2021, regardless of whether they received intravenous alteplase, were collected. To minimize technical deviation, four hospitals that met the criteria of being national senior stroke centers and had performed at least 60 cases annually for at least 2 years were selected. A data collection form was designed based on previous studies and included demographic characteristics, medical history, stroke etiology, vascular occlusion, EVT surgical procedures, the final modified Thrombolysis in Cerebral Infarction (mTICI) score, key time points, laboratory test results, symptomatic intracerebral hemorrhage (sICH), antiplatelet drugs administered after 24 hours, blood pressure parameters, and other relevant information. To ensure data quality, four specialized personnel were trained and divided into two groups, with each group independently completing the data collection. Patients with posterior circulation infarction, time from symptom onset to treatment > 4.5 hours, and endovascular treatment with intravenous alteplase were excluded. Data were thoroughly checked for accuracy and completeness, and patients were excluded if necessary. Finally, 204 participants within the 4.5-hour time window who received direct EVT were identified, with 102 patients treated with tirofiban and 102 patients not treated with tirofiban.
Inclusion and Exclusion Criteria
Based on clinical guidelines, we formulated appropriate inclusion and exclusion criteria. The inclusion criteria were patients who 1) were age ≥ 18 years; 2) were treated within 4.5 hours from onset; 3) had experienced an AIS induced by LVO, including the anterior cerebral artery (A1/A2) and middle cerebral artery (MCA; M1/M2), as confirmed by CT angiography and CT perfusion; 4) had received EVT regardless of the surgical procedure performed; and 5) had completed 90 days of follow-up. The exclusion criteria were patients who 1) had received intravenous thrombolysis prior to EVT; 2) had a malignant tumor with a short survival period; 3) had incomplete data; 4) were lost to follow-up; 5) had severe heart, lung, and renal disease combined with failure of ≥ 2 organs; and 6) had a prestroke modified Rankin Scale (mRS) score > 2.
Tirofiban Administration
We adhered to the established protocol for tirofiban use and dosage, as detailed in prior research.18Specifically, it is widely accepted that tirofiban should be administered immediately after endovascular treatment via continuous intravenous infusion at a rate of 0.1 μg/kg/min for a period of 12–24 hours following a low-dose intra-arterial bolus injection (0.25–1 mg) (Supplemental Fig. 1). Intraoperative evaluation guided the use of tirofiban in the following situations: 1) there was a high risk of reocclusion due to severe atherosclerosis; 2) successful recanalization was achieved at least 3 times, which resulted in endothelial damage or instant reocclusion; and 3) emergency stenting or balloon angioplasty for severe residual stenosis was received. Head CT was routinely performed at 4 hours and/or 24 hours after surgery, and oral antiplatelet treatment (one or two antiplatelet drugs according to guidelines) was prescribed.
Outcome Measures
The primary outcome of this study was the functional outcome attained at 90 days posttreatment, defined as an mRS score of 0–2 for a favorable functional outcome or an mRS score of 3–6 for an unfavorable functional outcome.1990天的夫人分数是通过teleph决定的one interviews conducted by trained personnel specialized in the management and follow-up of stroke patients. The secondary outcomes of the study included the incidence of sICH within 24 hours after EVT, successful recanalization after EVT as defined by an mTICI score of 2b or 3,20and mortality at 90 days.
The diagnosis of sICH was based on previously described criteria:211) a National Institutes of Health Stroke Scale (NIHSS) score that had increased > 4 points more than the previous score, 2) an NIHSS score that had increased at least 2 points in one category, and 3) unexplained neurological deterioration.
Statistical Analysis
One-way ANOVA was applied to analyze the baseline characteristics when the continuous variables and ordinal variables were in accordance with normal distribution. Otherwise, the Mann-Whitney U-test was used to analyze data, and these variables are presented as median and interquartile range. Categorical variables were analyzed by the chi-square test and are presented as percentages. For multivariate analysis, logistic regression was performed to adjust for some potential confounders with p < 0.2 in univariate analysis; these included sex, NIHSS score, age, hypertension, coronary artery disease, smoking history, drinking history, previous stroke history, mean arterial pressure within 24 hours, time from puncture to reperfusion, time from admission to reperfusion, time from onset to reperfusion, number of thrombectomy device passes, admission blood glucose, aspartate aminotransferase, infection, and myocardial infarction. SPSS version 25.0 software (IBM Corp.) was used for statistical analyses. A p value < 0.05 was considered statistically significant.
Results
Baseline Characteristics
In this retrospective study, we included 722 patients who underwent EVT for AIS between January 2020 and December 2021. Among them, 204 patients met the inclusion and exclusion criteria and were included in the study (Fig. 1). We conducted an analysis of the variables that may affect the prognosis of the patients, as shown inSupplemental Table 1. We found that factors such as tirofiban, admission NIHSS score, admission blood glucose, and infection were associated with the functional independence of the patients, as determined by logistic regression analysis (Supplemental Table 2).

Flowchart of patient selection.
Table 1presents a comparison between the tirofiban group and nontirofiban group, revealing that the former tended to consist of younger patients (median age 69.5 years in the tirofiban group vs 72.5 years in the nontirofiban group, p = 0.02) and a higher proportion of males (71.6% in the tirofiban group vs 54.9% in the nontirofiban group, p = 0.014) while showing lower rates of atrial fibrillation (35.3% in the tirofiban group vs 51.0% in the nontirofiban group, p = 0.024) and coronary heart disease (4.9% in the tirofiban group vs 14.7% in the nontirofiban group, p = 0.019), as well as a higher proportion of dual antiplatelet therapy (57.8% in the tirofiban group vs 33.3% in the nontirofiban group, p = 0.004). Conversely, the key quality control indicators, including time from admission to reperfusion (155 minutes in the tirofiban group vs 130 minutes in the nontirofiban group, p = 0.002), time from puncture to reperfusion (95 minutes in the tirofiban group vs 72 minutes in the nontirofiban group, p = 0.039), and time from onset to reperfusion (355 minutes in the tirofiban group vs 300 minutes in the nontirofiban group, p = 0.005), were significantly shorter in the nontirofiban group.
Baseline characteristics of patients in the tirofiban and nontirofiban groups
| Characteristic | Tirofiban (n = 102) | Nontirofiban (n = 102) | p Value |
|---|---|---|---|
| Age, yrs | 69.5 (57–76) | 72.5 (65.8–80.0) | 0.020* |
| Admission NIHSS score | 13 (10–17) | 14 (10–22.25) | 0.122 |
| Sex | 0.014* | ||
| Male | 73 (71.6) | 56 (54.9) | |
| Female | 29 (28.4) | 46 (45.1) | |
| Vascular risk factors | |||
| Hypertension | 69 (67.6) | 67 (65.7) | 0.766 |
| Diabetes | 29 (28.4) | 21 (20.6) | 0.193 |
| Atrial fibrillation | 36 (35.3) | 52 (51.0) | 0.024* |
| Smoking | 20 (19.6) | 15 (14.7) | 0.353 |
| Drinking | 11 (10.8) | 10 (9.8) | 0.818 |
| Coronary artery disease | 5 (4.9) | 15 (14.7) | 0.019* |
| Previous stroke | 23 (22.5) | 16 (15.7) | 0.213 |
| Occlusion sites | 0.165 | ||
| MCA | 68 (66.7) | 77 (75.5) | |
| ICA | 34 (33.3) | 25 (24.5) | |
| Stroke etiology | 0.454 | ||
| Large-artery atherosclerosis | 32 (31.4) | 24 (23.5) | |
| Cardioembolic | 58 (56.9) | 65 (63.7) | |
| Tandem lesion | 12 (11.8) | 13 (12.7) | |
| Treatments | |||
| Time from onset to hospital, mins | 180 (112.5–220) | 150 (120–240) | 0.960 |
| Time from onset to endovascular treatment, mins | 214 (150–300) | 210 (150–271.25) | 0.645 |
| Time from admission to reperfusion, mins | 155 (119.8–245.5) | 130 (93.75–192.5) | 0.002** |
| Time from admission to puncture, mins | 60 (25–101.3) | 40 (25–90) | 0.243 |
| Time from puncture to reperfusion, mins | 95 (49.8–140) | 72 (48–106.25) | 0.039* |
| Time from onset to reperfusion, mins | 355 (253.8–421.3) | 300 (235.75–360) | 0.005** |
| No. of thrombectomy device passes | 2 (1–3) | 2 (1–3) | 0.822 |
| Surgical procedure | |||
| Stent retriever & aspiration | 71 (69.6) | 94 (92.2) | <0.001*** |
| Stent retriever & aspiration w/ balloon angioplasty | 13 (12.7) | 2 (2.0) | |
| Stent retriever & aspiration w/ intracranial stenting | 8 (7.8) | 4 (3.9) | |
| Others† | 10 (9.8) | 2 (2.0) | |
| Blood pressure parameters, mm Hg | |||
| Admission systolic pressure | 134 (121.5–152.3) | 140 (130–150) | 0.393 |
| Admission diastolic pressure | 81.5 (70–94) | 80.5 (71.25–90) | 0.655 |
| Intraop systolic pressure | 140 (120–165) | 136 (120–155.25) | 0.312 |
| Intraop diastolic pressure | 80 (70–86.8) | 80 (70–87.25) | 0.798 |
| Intraop mean arterial pressure | 101.5 (88–108.3) | 99.5 (90–108.3) | 0.661 |
| Systolic pressure w/in 24 hrs | 128 (112.5–135) | 128 (118–143.25) | 0.242 |
| Diastolic pressure w/in 24 hrs | 74 (66–82.5) | 75 (63–84) | 0.954 |
| Mean arterial pressure w/in 24 hrs | 91 (81.8–99.2) | 92.8 (83–102.2) | 0.513 |
| Antiplatelet drugs after 24 hrs | |||
| Aspirin | 17 (16.7) | 33 (32.4) | 0.004** |
| Clopidogrel | 7 (6.9) | 7 (6.9) | |
| Aspirin+clopidogrel | 59 (57.8) | 34 (33.3) | |
| Surgical complications | |||
| sICH | 16 (15.7) | 17 (16.7) | 0.849 |
| Contrast medium leak | 17 (16.7) | 14 (13.7) | 0.558 |
| Reperfusion injury | 31 (30.4) | 35 (34.3) | 0.549 |
| Other events | |||
| Infection | 60 (58.8) | 56 (54.9) | 0.572 |
| Myocardial infarction | 6 (5.9) | 6 (5.9) | >0.999 |
| Laboratory test | |||
| ALT, U/L | 21.9 (13–27.7) | 19 (11.7–27) | 0.338 |
| AST, U/L | 22.8 (17–29.7) | 22.6 (17.1–29.8) | 0.870 |
| Admission blood glucose, mmol/L | 6.8 (5.4–8.5) | 6.8 (5.5–8.9) | 0.430 |
| Creatinine, μmol/L | 68 (56.5–83.2) | 64.9 (51.7–77.0) | 0.140 |
ALT = alanine transaminase; AST = aspartate aminotransferase; ICA = internal carotid artery.
Values are given as median (IQR) or number of patients (%) unless otherwise indicated.
p < 0.05; **p < 0.01; ***p < 0.001.
Stent retriever and aspiration with balloon angioplasty and intracranial stenting.
In this study, patients were classified into four subgroups based on the surgical procedure performed, which included stent retriever and aspiration, stent retriever and aspiration with balloon angioplasty, stent retriever and aspiration with intracranial stenting, and other compound procedures. The findings revealed that the majority of patients received a stent retriever and aspiration, with a rate of 92.2% in the nontirofiban group. Conversely, the rates of the other three surgical procedures, including balloon angioplasty, intracranial stenting, and other compound procedures, were higher in the tirofiban group than in the nontirofiban group. This suggests the presence of more local stenosis of the great vessels or in situ stenosis in the tirofiban group.
Association of Functional Independence With AIS and Anterior Circulation Vessel Occlusion
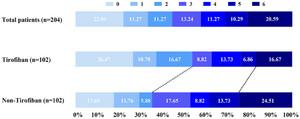
招募的204名患者的研究, 91 patients (44.6%) attained functional independence at 90 days as assessed by mRS scores of 0–2 (Fig. 2). Furthermore, we conducted a comparative analysis to evaluate the effectiveness of tirofiban in conjunction with direct thrombectomy, and the results indicated that the combination of tirofiban and direct thrombectomy was associated with a higher rate of favorable outcomes at 90 days. Specifically, in the tirofiban group, 55 patients (53.92%) achieved favorable outcomes, which was higher than the rate for the nontirofiban group, where only 35.29% of patients obtained favorable outcomes at 90 days. These findings suggest that the use of tirofiban in combination with direct thrombectomy may lead to improved clinical outcomes and could serve as a promising therapeutic option for patients undergoing direct thrombectomy.

Distribution of 90-day mRS scores of all patients who received direct thrombectomy for acute anterior circulation occlusion (upper). Distribution of 90-day mRS scores of patients who received tirofiban after direct thrombectomy (center). Distribution of 90-day mRS scores of patients who did not receive tirofiban after direct thrombectomy (lower).
Furthermore, after adjusting for various factors such as age, sex, atrial fibrillation, coronary artery disease, blood pressure parameters, antiplatelet drug use after 24 hours, surgical events, and laboratory test results, the logistic regression analysis demonstrated that the combination of tirofiban and direct thrombectomy was associated with a significant increase in the proportion of patients achieving mRS scores of 0–2 at 90 days (adjusted OR 0.429, 95% CI 0.207–0.888; adjusted p = 0.023) (Table 2). Additionally, the receiver operating characteristic curve analysis revealed that the area under the curve, sensitivity, and specificity were 0.826, 0.743, and 0.826, respectively (Fig. 3), which suggests that the logistic regression model has good accuracy in predicting the outcomes of interest.
Efficacy and safety endpoints of tirofiban in patients with direct thrombectomy for acute anterior circulation occlusion
| All Patients (n = 204) | Tirofiban (n = 102) | Nontirofiban (n = 102) | p Value | OR (95% CI) | Adjusted p Value | Adjusted OR (95% CI) | |
|---|---|---|---|---|---|---|---|
| mRS score 0 or 1 | 68 (33.3) | 38 (37.3) | 30 (29.4) | 0.235 | 1.425 (0.794 - -2.558) | 0.454 | 1.326 (0.634–2.776) |
| mRS score 0–2 | 91 (44.6) | 55 (53.9) | 36 (35.3) | 0.007** | 0.466 (0.266–0.818) | 0.023* | 0.429 (0.207–0.888) |
| Mortality | 42 (20.6) | 17 (16.7) | 25 (24.5) | 0.166 | 0.616 (0.309–1.227) | 0.286 | 0.604 (0.239–1.525) |
| Reperfusion injury | 66 (32.4) | 31 (30.4) | 35 (34.3) | 0.549 | 0.836 (0.464–1.504) | 0.669 | 0.855 (0.417–1.754) |
| sICH | 33 (16.2) | 16 (15.7) | 17 (16.7) | 0.849 | 0.930 (0.441–1.961) | 0.760 | 1.157 (0.454–2.951) |
Values are given as number of patients (%) unless otherwise indicated. Values were adjusted for sex, NIHSS score, age, hypertension, coronary artery disease, smoking history, drinking history, previous stroke history, mean arterial pressure within 24 hours, time from puncture to reperfusion, time from admission to reperfusion, time from onset to reperfusion, number of thrombectomy device passes, admission blood glucose, aspartate aminotransferase, infection, and myocardial infarction.
p < 0.05; **p < 0.01.

Receiver operating characteristic curve in the logistic regression model for the efficacy of tirofiban in patients undergoing direct thrombectomy for an acute anterior circulation occlusion. AUC = area under the curve.
sICH and 90-Day Mortality Rates
In order to determine the safety of tirofiban in conjunction with EVT for AIS, we evaluated the incidence of sICH and observed no significant differences between the tirofiban and nontirofiban groups (Table 1). This suggests that the use of tirofiban does not increase the risk of sICH in AIS patients undergoing EVT. Additionally, logistic regression analysis revealed that several factors, such as a history of stroke, admission blood glucose levels, elevated creatinine levels, and not taking antiplatelet drugs, may contribute to a higher mortality rate among patients undergoing EVT (Supplemental Table 3).
Furthermore, we examined the mortality rate as another safety indicator and observed that the mortality rate in the tirofiban group was only 16.67% (17/102), which was lower than the rate observed in the nontirofiban group (24.51%). These findings suggest that the application of low-dose tirofiban after direct thrombectomy is safe and may potentially reduce the mortality rate among AIS patients.
Beneficiaries of Tirofiban Combined With Direct Thrombectomy Treatment of AIS With Anterior Circulation Vessel Occlusion
We used a stratified analysis approach to investigate the influence of tirofiban on clinical outcomes by analyzing selected important variables, including age, sex, baseline NIHSS score, time from onset to reperfusion, site of occlusion, stroke etiology, and diabetes. We identified the median values for these variables and stratified the data accordingly. Our results suggest that male patients (adjusted OR 0.286, 95% CI 0.116–0.704) with an age > 72 years (adjusted OR 0.229, 95% CI 0.064–0.814), a baseline NIHSS score > 14 (adjusted OR 0.313, 95% CI 0.102–0.961), a medical history of diabetes (adjusted OR 0.089, 95% CI 0.011–0.743), and a time from onset to reperfusion > 327 minutes (adjusted OR 0.255, 95% CI 0.084–0.770) were more likely to benefit from tirofiban treatment (Fig. 4).

Correlation factors of 90-day functional independence scores of patients who received tirofiban in conjunction with direct thrombectomy for an acute anterior circulation occlusion. ICA = internal carotid artery; NA = not applicable.
Discussion
在这个多中心,双向comprisin学习g both retrospective (2020) and prospective (2021) data from China, we evaluated the efficacy and safety of tirofiban in acute cerebral infarction of the anterior circulation treated with EVT alone and with EVT with intravenous alteplase. Our findings revealed that tirofiban treatment after EVT could significantly improve functional independence compared with EVT alone. We further observed that male patients with a baseline NIHSS score > 14 and a medical history of diabetes were more likely to benefit from tirofiban. However, these results require validation through future randomized controlled trials.
In recent years, reducing the reocclusion rate after EVT in AIS has emerged as an effective strategy for improving functional independence. Glycoprotein IIb/IIIa antagonists are potential therapeutic agents that act as a bridge between EVT and oral antiplatelet drugs by suppressing thrombus growth and re-formation. Although eptifibatide combined with mechanical thrombectomy has shown a trend toward favorable outcomes, the difference was not statistically significant.11Intravenous abciximab may serve as a rescue therapy for immediate reocclusion after mechanical thrombectomy.12Among the glycoprotein IIb/IIIa antagonists, tirofiban is the antagonist predominantly used in cases of AIS.10As an adjunctive therapy to EVT, intra-arterial, intravenous, or low-dose tirofiban may be safe and effective in AIS patients due to its fast-acting antiplatelet effect. This study focuses on the effect of tirofiban on direct thrombectomy for anterior vessel occlusion and reveals its significant role in improving clinical prognosis.
In contrast to our study, the RESCUE BT and Direct-MT studies indicated that patients who received intravenous tirofiban before EVT for AIS induced by LVO within 24 hours of onset did not attain a favorable outcome compared with placebo treatment.13,21The differences between our study and the others are 1) the time of treatment (after EVT in ours vs before EVT in the others), 2) the time from onset to treatment (within 4.5 hours vs within 24 hours), and 3) the duration of treatment with tirofiban (continuous infusion for 12–24 hours vs up to 24 hours). These differences might provide a new perspective on the timing and duration of tirofiban treatment as well as a more reliable basis for future clinical RCT studies.
It is widely acknowledged that advanced age, higher NIHSS scores, medical history of diabetes, and longer time delays are closely linked to poor stroke prognosis, which may be attributed to complications such as reocclusion, severe inflammatory response, and reperfusion injury.22–25Therefore, physicians have been searching for effective interventions to improve AIS outcomes, with strategies aimed at blocking inflammation and inhibiting platelet aggregation to reduce the incidence of reocclusion and promote functional independence.26,27在这项研究中,我们发现选择性glycoprotein IIb/IIIa receptor antagonist tirofiban performed efficiently in direct thrombectomy for acute anterior circulation occlusion, particularly in patients with advanced age, higher admission NIHSS scores, delayed time from onset to reperfusion, and a medical history of diabetes. This result suggests that the more severe the illness, the greater the potential benefit patients may derive from tirofiban, possibly by inhibiting reocclusion.
Previous research has indicated that older patients and those with diabetes are more prone to acute thrombosis and reocclusion due to severe vascular endothelial injury, poor repair function, and increased thrombogenicity.28In addition, male patients treated with tirofiban have shown improved outcomes, although the reason behind this remains unclear.29The admission NIHSS score and a delayed time from onset to reperfusion have also been identified as negative predictors of clinical prognosis, with higher scores and longer delays associated with worse outcomes. In the case of anterior circulatory occlusion, NIHSS scores reflect the severity of vascular obstruction, and in this study, 71% (145/204) of patients had MCA lesions, which is consistent with the higher incidence of intracranial artery stenosis in the Chinese population.30Because intracranial artery stenosis is more prone to thrombosis, the administration of antiplatelet drugs immediately after thrombectomy may be effective and applicable in clinical practice.17Moreover, our analysis found that 58 (56.9%) of the cardioembolic stroke patients were treated with tirofiban and did not experience an increased risk of sICH. Furthermore, we investigated the effect of tirofiban in patients who received bridging therapy with intravenous thrombolysis prior to EVT and found that the nontirofiban group had a higher rate of favorable outcomes (mRS scores 0–2) than the tirofiban group (38.31% vs 47.47%) (Supplemental Fig. 2).
In summary, our findings suggest that the use of tirofiban following direct thrombectomy without bridging treatment may be both effective and safe for the treatment of anterior circulation vessel occlusion. This treatment approach may be particularly beneficial for male patients with advanced age, higher admission NIHSS scores, longer time delay from onset to reperfusion, and diabetes.
Limitations
The current study has several limitations that need to be considered when interpreting the results. First, the data were collected retrospectively and were not derived from a randomized controlled trial, which might affect the accuracy and generalizability of the findings. Second, the decision to administer tirofiban was made by the treating physicians based on the individual patient’s situation, which could introduce bias into the results. Third, the duration and maintenance of tirofiban administration varied among the patients in the study, which could affect the efficacy and safety of the treatment. Finally, there were significant differences of variables between the tirofiban and nontirofiban groups, including age, sex, medical history (atrial fibrillation and coronary artery disease), critical time points (time from admission to reperfusion, time from puncture to reperfusion, and time from onset to reperfusion), surgical procedures, and the selection of antiplatelet drugs 24 hours after the procedure, which may have influenced the clinical outcomes.
Conclusions
The combination of tirofiban and EVT for AIS with anterior circulation vessel occlusion has been shown to be both effective and safe. Although male patients with higher baseline NIHSS scores or diabetes tended to have better outcomes, further confirmation of these findings is necessary through randomized controlled trials.
Key Messages
What is already known on this topic? Although the glycoprotein IIb/IIIa antagonist tirofiban is widely used in AIS for suppressing thrombus growth and re-formation, its efficacy and safety remain controversial.
What does this study add? This study indicated that tirofiban treatment following EVT for AIS with anterior circulation vessel occlusion was effective and safe. Also, male patients with higher baseline NIHSS scores or diabetes had a tendency to benefit from tirofiban treatment.
How might this study affect research, practice, or policy? Tirofiban might be an effective treatment for reducing the reocclusion rate in patients with anterior circulation vessel occlusion who receive EVT.
Acknowledgments
我们承认所有参与中心和探讨tigators for helping with data collection. The following centers were involved: Nanjing First Hospital, Nanjing Medical University, Changzhou No. 2 People’s Hospital, and Subei People’s Hospital of Jiangsu Province. This work received funding from the Department of Human Resources and Social Security of Jiangsu Province | Key Medical Subjects of Jiangsu Province (BE2020620 to Y.X.) and the National Natural Science Foundation of China (82071304 and 81671149 to Q.Z.).
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author Contributions
Conception and design: Q Zhang, Guan, X Li, Zhou. Acquisition of data: Q Zhang, Guan, Ni, Lv, Xie. Analysis and interpretation of data: Q Zhang, Guan, X Li, Ni, Xie, J Li. Drafting the article: Q Zhang, Yun, L Zhang. Critically revising the article: Q Zhang, Guan, Yun, Xu. Reviewed submitted version of manuscript: Q Zhang, Yun, Xu. Approved the final version of the manuscript on behalf of all authors: Q Zhang. Statistical analysis: Q Zhang, X Li, J Li. Administrative/technical/material support: Q Zhang, Guan, X Li. Study supervision: Q Zhang, Zhou, Xu, J Li.
Supplemental Information
Online-Only Content
Supplemental material is available online.
Supplemental Figures and Tables.//www.prize-show.com/doi/suppl/10.3171/2023.7.FOCUS23150.
References
-
1 ↑
FeilK,MatuseviciusM,HerzbergM,et al.Minor stroke in large vessel occlusion: a matched analysis of patients from the German Stroke Registry-Endovascular Treatment (GSR-ET) and patients from the Safe Implementation of Treatments in Stroke-International Stroke Thrombolysis Register (SITS-ISTR).Eur J Neurol.2022;29(6):1619–1629.
-
2
KvistadCE,NæssH,HellebergBH,et al.Tenecteplase versus alteplase for the management of acute ischaemic stroke in Norway (NOR-TEST 2, part A): a phase 3, randomised, open-label, blinded endpoint, non-inferiority trial.Lancet Neurol.2022;21(6):511–519.
-
3 ↑
RoaldsenMB,LindekleivH,MathiesenEB.Intravenous thrombolytic treatment and endovascular thrombectomy for ischaemic wake-up stroke.Cochrane Database Syst Rev.2021;12(12):CD010995.
-
4 ↑
BenaliF,KappelhofM,OspelJ,et al.Benefit of successful reperfusion achieved by endovascular thrombectomy for patients with ischemic stroke and moderate pre-stroke disability (mRS 3): results from the MR CLEAN Registry.J Neurointerv Surg.2023;15:433–438.
-
5 ↑
LeischnerH,BrekenfeldC,MeyerL,et al.Study criteria applied to real life-a multicenter analysis of stroke patients undergoing endovascular treatment in clinical practice.J Am Heart Assoc.2021;10(22):e017919.
-
6 ↑
MartoJP,StramboD,HajduSD,et al.Twenty-four-hour reocclusion after successful mechanical thrombectomy: associated factors and long-term prognosis.Stroke.2019;50(10):2960–2963.
-
7
MosimannPJ,KaesmacherJ,GautschiD,et al.Predictors of unexpected early reocclusion after successful mechanical thrombectomy in acute ischemic stroke patients.Stroke.2018;49(11):2643–2651.
-
8 ↑
SubramanianA,DelaneyS,MurphySJX,et al.Platelet biomarkers in patients with atherosclerotic extracranial carotid artery stenosis: a systematic review.欧元J Vasc Endovasc杂志.2022;63(3):379–389.
-
9 ↑
WeiL,ZhaoWB,YeHW,et al.Heart rate variability in patients with acute ischemic stroke at different stages of renal dysfunction: a cross-sectional observational study.Chin Med J (Engl).2017;130(6):652–658.
-
10 ↑
YangJ,WuY,GaoX,et al.Intraarterial versus intravenous tirofiban as an adjunct to endovascular thrombectomy for acute ischemic stroke.Stroke.2020;51(10):2925–2933.
-
11 ↑
MaG,SunX,ChengH,et al.Combined approach to eptifibatide and thrombectomy in acute ischemic stroke because of large vessel occlusion: a matched-control analysis.Stroke.2022;53(5):1580–1588.
-
12 ↑
DelvoyeF,LoyauS,LabreucheJ,et al.Intravenous abciximab as a rescue therapy for immediate reocclusion after successful mechanical thrombectomy in acute ischemic stroke patients.Platelets.2022;33(2):285–290.
-
13 ↑
QiuZ,LiF,SangH,et al.Effect of intravenous tirofiban vs placebo before endovascular thrombectomy on functional outcomes in large vessel occlusion stroke: the RESCUE BT randomized clinical trial.JAMA.2022;328(6):543–553.
-
14
BaekBH,YoonW,LeeYY,KimSK,KimJT,ParkMS.Intravenous tirofiban infusion after angioplasty and stenting in intracranial atherosclerotic stenosis-related stroke.Stroke.2021;52(5):1601–1608.
-
15
TangL,TangX,YangQ.The application of tirofiban in the endovascular treatment of acute ischemic stroke: a meta-analysis.Cerebrovasc Dis.2021;50(2):121–131.
-
16
ZhaoW,CheR,ShangS,et al.Low-dose tirofiban improves functional outcome in acute ischemic stroke patients treated with endovascular thrombectomy.Stroke.2017;48(12):3289–3294.
-
17 ↑
ZhuF,AnadaniM,LabreucheJ,et al.Impact of antiplatelet therapy during endovascular therapy for tandem occlusions: a collaborative pooled analysis.Stroke.2020;51(5):1522–1529.
-
18 ↑
HuoX,YangM,MaN,et al.Safety and efficacy of tirofiban during mechanical thrombectomy for stroke patients with preceding intravenous thrombolysis.Clin Interv Aging.2020;15:1241–1248.
-
19 ↑
van SwietenJC,KoudstaalPJ,VisserMC,SchoutenHJ,van GijnJ.Interobserver agreement for the assessment of handicap in stroke patients.Stroke.1988;19(5):604–607.
-
20 ↑
ZaidatOO,YooAJ,KhatriP,et al.Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement.Stroke.2013;44(9):2650–2663.
-
21 ↑
ZhangY,ZhangL,ZhangY,et al.Endovascular recanalization for acute internal carotid artery terminus occlusion: a subgroup analysis from the Direct-MT trial.开云体育app官方网站下载入口.2022;91(4):596–603.
-
22 ↑
MistryEA,YeattsS,de HavenonA,et al.Predicting 90-day outcome after thrombectomy: baseline-adjusted 24-hour NIHSS is more powerful than NIHSS score change.Stroke.2021;52(8):2547–2553.
-
23
HuG,PanY,WangM,et al.Inverse association between high-density lipoprotein cholesterol and adverse outcomes among acute ischemic stroke patients with diabetes mellitus.Biomedicines.2021;9(12):1947.
-
24
DongN,ShenX,WuX,GuoX,FangQ.Elevated glycated hemoglobin levels are associated with poor outcome in acute ischemic stroke.Front Aging Neurosci.2022;13(13):821336.
-
25 ↑
GogelaSL,GozalYM,ZhangB,et al.Severe carotid stenosis and delay of reperfusion in endovascular stroke treatment: an Interventional Management of Stroke-III study.J Neurosurg.2018;128(1):94–99.
-
26 ↑
LiX,LinS,ChenX,et al.The prognostic value of serum cytokines in patients with acute ischemic stroke.Aging Dis.2019;10(3):544–556.
-
27 ↑
PandhiA,TsivgoulisG,KrishnanR,et al.Antiplatelet pretreatment and outcomes following mechanical thrombectomy for emergent large vessel occlusion strokes.J Neurointerv Surg.2018;10(9):828–833.
-
28 ↑
WolfV,AbdulY,LiW,ErgulA.糖尿病和缺血性中风的蜡膜的影响brovasculature: a female perspective.Neurobiol Dis.2022;167:105667.
-
29 ↑
WangM,WangC,GuHQ,et al.Sex differences in short-term and long-term outcomes among acute ischemic stroke patients in China.Stroke.2022;53(7):2268–2275.
-
30 ↑
LiS,FangF,CuiM,et al.Incidental findings on brain MRI among Chinese at the age of 55–65 years: the Taizhou Imaging Study.Sci Rep.2019;9(1):464.