Thesuperficial temporal artery–middle cerebral artery (STA-MCA) bypass was introduced more than 50 years ago, and the craft involved in bypass surgery remains simple, with surgeons relying on suturing and basic instruments, three different types of anastomoses, minimal technology, and manual dexterity. Nonetheless, creative neurosurgeons have advanced bypass surgery into a complex surgical art by developing an array of bypasses that include standard extracranial-to-intracranial (EC-IC) bypass using scalp arteries, EC-IC with interpositional grafts, and intracranial-to-intracranial (IC-IC) bypass to reimplant, reanastomose, and communicate with cerebral arteries without the use of EC donors and sometimes with the use of IC jump grafts.1–8Bypass surgery has also evolved through the use of a variety of donor arteries, recipient arteries, interpositional grafts, anastomoses, and suturing techniques. Despite inherent anatomical and technical limitations, bypass surgery is one of only a few constructive rather than deconstructive procedures in neurosurgery, and it fosters innovation. The literature is full of bypass inventions that adapt a patient’s unique arterial anatomy to revascularize brain tissue after trapping, occluding, or obliterating vascular pathology.9–23
Although the levels of innovation, technical skill, and complexity evident in contemporary bypasses have increased, the literal descriptions of these new bypasses have not kept pace. A system of symbols has been developed to sketch bypasses,3and although this system is valuable in the context of a textbook,24其广泛的应用程序通信ns and publications is difficult to achieve. Most bypasses are written as the names of the donor and recipient arteries joined with a hyphen, as in the prototypical STA-MCA bypass. These descriptions are simplistic, underinformative, and inadequate. For example, the STA-MCA bypass is usually constructed with an end-to-side anastomosis to a corticalM4branch through a small frontotemporal craniotomy. However, it might also be constructed with an end-to-end anastomosis to an insularM2branch deep in thesylvian fissurethrough a pterional craniotomy. Proper bypass nomenclature should capture these differences in construction and technique.
现有的术语往往是模糊和may even be inaccurate. Therefore, an updated, improved system is needed. In descriptions of cerebral bypasses, donor and recipient arteries are essential and form the basis of the current nomenclature, but fundamental elements are missing, such as segmental anatomy, or the “address” of the bypass; the type of anastomosis (end-to-side, end-to-end, or side-to-side); and any special techniques, like extraluminal versus intraluminal suturing. Other descriptors, like left- and right-sidedness and the type of interpositional graft, should also be included. A better bypass nomenclature would include all of these missing elements to enable a complete description of bypass construction. In contrast to that of previous systems, we propose a method that uses an alphanumeric code that can describe specific bypasses more quickly and without drawings because the descriptive elements are systematically incorporated with alphanumeric abbreviations. We have sought to make this code for bypass surgery terminology clear, concise, and unambiguous to offer an easy shorthand for complex operations. We have found the proposed nomenclature to be simple, practical, and easy to learn, and its use may enhance understanding of bypass procedures, clarify important technical nuances, and improve communications and publications.
开云体育世界杯赔率
Proposed Nomenclature for Cerebral Bypasses
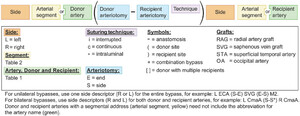
In its simplest form, a bypass consists of a donor artery and a recipient artery, the anastomosis that joins them, and left- or right-sidedness. Therefore, in the proposed system, the basic code consists of side (right or left), arterial segment, and arteriotomy in the anastomosis for both the donor and recipient arteries (Fig. 1).The most important details are the specific anatomical locations of the bypass donor and recipient sites, which require abbreviations for the parent artery (e.g., external carotid artery [ECA] orpericallosal artery[PcaA]) (Table 1) and one of the main cerebral or cerebellar arteries for the segmental address (e.g., M2, A3, s1) (Table 2,Fig. 2).Alphanumeric descriptions of segmental anatomy were established by Rhoton and colleagues for cerebral arteries in uppercase25and by Lawton and colleagues for cerebellar arteries in lowercase.26In the proposed nomenclature, parent artery abbreviations with a segmental address are redundant and are therefore excluded to simplify the code. For example, an M4MCArecipient artery would be described only as M4 in the standard bypass nomenclature for moyamoya disease. Branch arteries, or those without a segmental address, are described with the parent artery abbreviations. The donor artery precedes the recipient artery in the nomenclature, reflecting the direction of anterograde blood flow in the bypass.

Formula for cerebral bypass coding. Each artery involved in a bypass is codified by four primary elements: the side, an arterial segment, an arterial abbreviation, and an arteriotomy. Donor and recipient sites with a segmental address need not include the corresponding arterial abbreviation. Donor and recipient sites without a segmental address require an arterial abbreviation. The parentheses and a hyphen group the arteriotomies that are sutured together in the anastomosis. A fifth element denotes the suturing technique; for example, the asterisk (*) indicates an intraluminal suturing technique. Please refer toTables 1and2for the lists of artery and segment abbreviations, respectively, used in all of the figures.
Abbreviations for cranial arteries used in bypass procedures for the proposed nomenclature
| Abbreviation | Artery Name |
|---|---|
| ACA | Anterior cerebral artery |
| AChA | Anterior choroidal artery |
| ACoA | Anterior communicating artery |
| AICA | Anterior inferior cerebellar artery |
| AIFA | Anterior internal frontal artery |
| AngA | Angular artery |
| APA | Anterior parietal artery |
| ATA | Anterior temporal artery |
| BA | Basilar artery |
| CalcA | Calcarine artery |
| CenA | Central artery |
| CmaA | Callosomarginal artery |
| ECA | External carotid artery |
| FPA | Frontopolar artery |
| fSTA | Frontal branch of STA |
| ICA | Internal carotid artery |
| IMA | Internal maxillary artery |
| InfTr | Inferior trunk of MCA |
| IPA | Inferior parietal artery |
| MCA | Middle cerebral artery |
| MidTr | Middle trunk of MCA |
| MMA | Middle meningeal artery |
| MTA | Middle temporal artery |
| OFA | Orbitofrontal artery |
| OphA | Ophthlamic artery |
| PAA | Posterior auricular artery |
| PCA | Posterior cerebral artery |
| PcaA | Pericallosal artery |
| PCenA | Paracentral artery |
| PCoA | Posterior communicating artery |
| PFA | Prefrontal artery |
| PICA | Posterior inferior cerebellar artery |
| PIFA | Posterior internal frontal artery |
| POA | Parieto-occipital artery |
| PoCenA | Postcentral artery |
| PPA | Posterior parietal artery |
| PrCenA | Precentral artery |
| pSTA | Parietal branch of STA |
| PTA | Posterior temporal artery |
| RAH | Recurrent artery of Heubner |
| SCA | Superior cerebellar artery |
| SPA | Superior parietal artery |
| STA | Superficial temporal artery |
| SupTr | Superior trunk of MCA |
| TOA | Temporo-occipital artery |
| TPA | Temporopolar artery |
| VA | Vertebral artery |
Abbreviations for arterial segments of intracranial arteries for the proposed nomenclature (segmental addresses)
| Segment Number | Artery | Segment Name |
|---|---|---|
| C1 | ICA | Cervical |
| C2 | ICA | Petrous |
| C3 | ICA | Lacerum |
| C4 | ICA | Cavernous |
| C5 | ICA | Clinoidal |
| C6 | ICA | Ophthalmic |
| C7 | ICA | Communicating |
| A1 | ACA | Precommunicating or horizontal |
| A2 | ACA | Postcommunicating or infracallosal |
| A3 | ACA | Precallosal |
| A4 | ACA | Supracallosal |
| A5 | ACA | Postcallosal |
| M1 | MCA | Sphenoidal |
| M2 | MCA | Insular |
| M3 | MCA | Opercular |
| M4 | MCA | Cortical |
| P1 | PCA | Precommunicating |
| P2 | PCA | Postcommunicating |
| P2A | PCA | Crural |
| P2P | PCA | Ambient |
| P3 | PCA | Quadrigeminal |
| P4 | PCA | Calcarine |
| s1 | SCA | Anterior pontomesencephalic |
| s2 | SCA | Lateral pontomesencephalic |
| s3 | SCA | Cerebellomesencephalic |
| s4 | SCA | Cortical |
| a1 | AICA | Anterior pontine |
| a2 | AICA | Lateral pontine |
| a3 | AICA | Flocculopeduncular |
| a4 | AICA | Cortical |
| p1 | PICA | Anterior medullary |
| p2 | PICA | Lateral medullary |
| p3 | PICA | Tonsillomedullary |
| p4 | PICA | Telovelotonsillar |
| p5 | PICA | Cortical |

Schematic representation of MCA (left side) and ACA (right side) bypasses. CCA = common carotid artery; ICA = internal carotid artery; OA = occipital artery. Modified with permission from Thieme Medical Publishers from Lawton MT.Seven Bypasses: Tenets and Techniques for Revascularization. New York: Thieme; 2018.
In the proposed system, the hyphen continues to be used to depict the anastomosis connecting donor and recipient arteries. However, three different types of anastomoses join donor and recipient arteries, and this anastomotic detail is incorporated in the nomenclature by adding an abbreviation for the position of the arteriotomy (end [E], side [S]) on each side of the hyphen for the different anastomoses: end-to-side (E-S), end-to-end (E-E), or side-to-side (S-S). Sidedness (right [R] or left [L]) is included as a prefix to avoid having the anastomotic detail in the middle of the code. For example, the superficial STA-MCA bypass becomes the L STA (E-S) M4 bypass. Bypasses that are unilateral use one descriptor for the entire bypass, whereas bypasses that are bilateral need descriptors for both donor and recipient. For theposterior inferior cerebellar artery(PICA), for example, the PICA-PICA bypass between the caudal loops of the tonsillomedullary segments would be L p3 (S-S) R p3 bypass, with the flow in the completed construct coursing from left to right.
More complex bypasses have additional details and conventions. Interpositional bypasses require the description of the graft, which is typically a radial artery graft (RAG) or saphenous vein graft (SVG) but may also include other elements, such as the posterior tibial artery or lateral circumflex femoral artery. Interpositional grafts are inserted between donor and recipient abbreviations and are joined by the applicable anastomotic abbreviation, for example, R ECA (S-E) RAG (E-S) M2 bypass.
Combination bypasses are constructs with multiple anastomoses indicated by the use of the + sign. For example, a double-barrel STA-MCA bypass from the frontal branch of the STA (fSTA) and parietal branch of the STA (pSTA) to the superior and inferior trunks of an MCA bifurcation aneurysm would be described as R fSTA (E-S) M2 + pSTA (E-S) M2´, with a prime symbol used to denote a second and different M2 MCA recipient.
More complex combination bypasses require brackets positioned according to the mathematical distributive property, by which multiplying the sum of two or more addends by a number equals adding the products of each addend multiplied by the number individually: a × [b + c] = [a × b] + [a × c]. Similarly, with bypass code, a donor artery that supplies two recipients can be described with brackets and addition. For example, a double reimplantation bypass that revascularizes the superior and inferior trunks of an MCA bifurcation aneurysm with one high-flow graft from the left cervical carotid artery would be L ECA (S-E) RAG [(S-E) M2 + (E-S) M2´].
An additional detail is the type of suturing technique used. Bypasses are sewn with either interrupted or continuous sutures. In addition, most suture lines are sewn extraluminally but occasionally must be sewn intraluminally due to immobility of the arteries or other reasons. For example, the deep suture line of an S-S bypass ("in situ bypass") is sewn with running intraluminal suturing, and occasionally this technique is applied to the E-E and E-S anastomoses.27这些缝合技术细节可以添加到the nomenclature with superscripts within the anastomotic parentheses: “i” for interrupted, “c” for continuous, and “*” for intraluminal suturing technique. In the previous example, L ECA (S-E) RAG [(S-E) M2 + (E-S) M2´], this detail would be incorporated as follows: L ECA (S-Ec) RAG [(S-Ec*) M2 + (E-Sc*) M2´].
Literature Review
英文医学文献回顾ed using the PubMed database to search for combinations of the following keywords: “cerebral revascularization,” “cerebral bypass,” “intracranial,” “extracranial,” “aneurysm,” “vascular insufficiency,” and “complex,” which yielded 3643 articles. Articles using descriptions of bypasses were included and reviewed for incompleteness or ambiguity in the authors’ descriptive abbreviations. Cross-referencing was then performed to find any missing articles.
Bypass nomenclature found in the literature was categorized into four distinct groups as follows. A bypass was categorized as complete (C) if the nomenclature described the donor artery, recipient artery, segmental arterial anatomy, sidedness, interpositional graft (if any), and the type of anastomoses. A bypass described only by the donor and recipient arteries without any additional detail was categorized as donor-recipient (D-R; e.g., STA-MCA). A bypass described by the donor and recipient arteries with some additional details, such as the sidedness, the graft, or the segmental anatomy of the involved arteries, but without complete detail, was categorized as “donor-recipient plus” (D-R+; e.g., STA-M4 MCA bypass). A bypass described by less information than the donor and recipient arteries was categorized as donor-recipient minus (D-R−; e.g., STA bypass). A bypass described by a unique adjective or coined term was categorized as ambiguous (A; e.g., azygos bypass, bonnet bypass, or arborization bypass).21,28–34Finally, a bypass described with detailed text for steps from beginning to end of the procedure was categorized as descriptive text (DT).
Results
Of the 3643 publications identified in the PubMed search, 483 were found that included at least one description of a cerebral bypass. STA-MCA bypass was the bypass described most frequently (62%). Most bypass descriptions were categorized into the D-R group (335 D-R, 69%). D-R+ descriptions with additional details were reported in 97 papers (20%), and D-R− descriptions with fewer details were reported in 56 papers (12%). No publication contained a complete description of a bypass. The bypasses in 45 articles (9.3%) were categorized as A (ambiguous), and in 135 articles (21.5%), bypasses were described with DT.
We were able to apply the proposed nomenclature to some of the most colorful and complex bypasses in the literature (Fig. 3A).Russin also described an “arborization” bypass to revascularize a fusiform M2 MCA aneurysm incorporating the origin of two temporalM3(tM3) branches.9使用的树枝状连续两个s anastomoses, the first between an fM3 and one of the temporal branches, and the second between the two temporal branches at a point distal to the first anastomosis. The proposed nomenclature describes this bypass as L fM3 (S-S) tM3 + tM3 (S-S) tM3´. This combination bypass is indicated by the plus (+) sign. The M3´ indicates an M3 branch different from the branch involved in the S-S anastomosis between the temporal and frontal branches, and the prime symbol is used because these opercular segments lack distinct names.

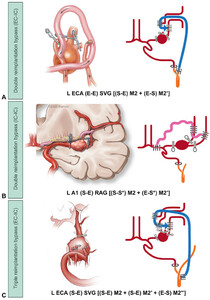
Descriptions of complex bypasses with illustrations, symbol schematics (seeFig. 2for the key), and proposed alphanumeric coding.A:Arborization bypass in the ACA territory: L CmaA (S-S*) R CmaA + L PcaA (S-S*) R PcaA.B:YSTA interpositional bypass in the ACA territory: L A2 (S-E) YSTA [(E-S) L A3 + (E-S) R A3].C:Bonnet bypass: L STA (S-E) SVG (E-S*) R M2. Panels A left and C left published with permission from Barrow Neurological Institute, Phoenix, AZ. Panel B left from Endo H, Sugiyama SI, Endo T, et al. Revascularization of the anterior cerebral artery by Y-shaped superficial temporal artery interposition graft for the treatment of a de novo aneurysm arising at the site of A3-A3 bypass: technical case report.J Neurosurg. 2018;129(5):1120–1124. © 2018 Hidenori Endo; published with permission. Panels A right, B right, and C right modified with permission from Thieme Medical Publishers from Lawton MT.Seven Bypasses: Tenets and Techniques for Revascularization. New York: Thieme; 2018.
The double-limbed bypass uses a Y-shaped interpositional graft from a harvested STA trunk and its frontal and parietal branches (Fig. 3B).Endo et al. used a Y-shaped STA graft (YSTA) to revascularize a complexanterior communicating artery(ACoA) aneurysm, connecting a single proximal A2anterior cerebral artery(ACA) donor and two bilateral A3 ACA recipients: L A2 (S-E) YSTA [(E-S) L A3 + (E-S) R A3].35The brackets denote a combination bypass with two distal anastomoses supplied by a single graft. An RAG may also be refashioned into a Y-shaped graft (YRAG) to create a similar bypass.36The “bonnet bypass” reported by Spetzler et al. is a construct that connects a contralateral STA donor to an ipsilateral MCA via a long graft over the convexity of the brain (Fig. 3C).37The proposed nomenclature can readily capture different bonnet bypasses, for example, R STA (S-E) SVG (E-S) L M4.
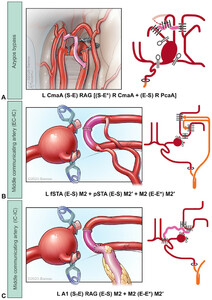
Lawton and Quiñones-Hinojosa introduced double reimplantation bypass for reconstructing bifurcations after aneurysm trapping using a single nonbranched graft to supply two recipient arteries.38The graft is connected proximally to the donor artery, and efferent branches are then reimplanted onto the graft with each subsequent anastomosis. This technique was first introduced as an EC-IC interpositional bypass: L ECA (E-E) SVG [(S-E) M2 + (E-S) M2´] (Fig. 4A).The double bypass technique then evolved to include an IC-IC interpositional bypass with the use of theA1ACA as an intracranial donor site: L A1 (S-E) RAG [(S-S) M2 + (E-S) M2´] (Fig. 4B).这种技术发展进一步包括一个“佛urth-generation” IC-IC interpositional bypass with the use of intraluminal suturing for the reimplanted MCA trunks: R A1 (S-Ec) SVG [(S-Sc*) M2 + (E-Sc*) M2´]; the bypass may also be constructed with an RAG. The first reimplantation is an S-S anastomosis, and the second reimplantation uses intraluminal suturing to sew the deep suture line, both denoted with asterisks in the code (Fig. 4B).The double bypass technique may be similarly used for a triple bypass: L ECA (S-E) SVG [(S-E) M2 + (S-E) M2´ + (Ε-S) M2´´] (Fig. 4C).

Descriptions of complex bypasses with illustrations, symbol schematics (seeFig. 2for the key), and proposed alphanumeric coding.A:Double reimplantation technique, EC-IC: L ECA (E-E) SVG [(S-E) M2 + (E-S) M2´].B:Double reimplantation technique, IC-IC: L A1 (S-E) RAG [(S-S*) M2 + (E-S*) M2´].C:Triple reimplantation technique, EC-IC: L ECA (S-E) SVG [(S-E) M2 + (S-E) M2´ + (E-S) M2´´]. Panel A left published with permission from Lawton MT, Quiñones-Hinojosa A. Double reimplantation technique to reconstruct arterial bifurcations with giant aneurysms.开云体育app官方网站下载入口. 2006;58(4)(suppl 2):ONS-347–ONS-354. By permission of the Congress of Neurological Surgeons. Panel B left published with permission from Barrow Neurological Institute, Phoenix, AZ. Panel C left reprinted by permission from Springer Nature:Acta Neurochir. Wessels L, Fekonja LS, Vajkoczy P. Bypass surgery of complex middle cerebral artery aneurysms—technical aspects and outcomes. © Springer-Verlag GmbH Austria 2019;161:1981–1991. Panels A right, B right, and C right modified with permission from Thieme Medical Publishers from Lawton MT.Seven Bypasses: Tenets and Techniques for Revascularization.New York: Thieme; 2018.
The azygos bypass is a double reimplantation bypass in the ACA territory with construction similar to that used in the treatment of a giant, thrombotic ACoA aneurysm.11The name is ambiguous, but its code provides the complete details for azygos bypass construction, including thecallosomarginal artery(CmaA): R PcaA (S-Ec) RAG [(S-Sc*) L PcaA + (E-Sc) L CmaA]. A different example of an azygos bypass is shown inFig. 5A, and its details are captured completely by the code: L CmaA (S-E) RAG [(S-E*) R CmaA + (E-S) R PcaA].

Descriptions of complex bypasses with illustrations, symbol schematics (seeFig. 2for the key), and proposed alphanumeric coding.A:Azygos bypass: L CmaA (S-E) RAG [(S-E*) R CmaA + (E-S) R PcaA].B:MCoA, EC-IC: L fSTA (E-S) M2 + pSTA (E-S) M2´ + M2 (E-E*) M2´.C:MCoA, IC-IC: L A1 (S-E) RAG (E-S) M2 + M2 (E-E*) M2´. Panels A left, B left, and C left published with permission from Barrow Neurological Institute, Phoenix, AZ. Panels A right, B right, and C right modified with permission from Thieme Medical Publishers from Lawton MT.Seven Bypasses: Tenets and Techniques for Revascularization. New York: Thieme; 2018.
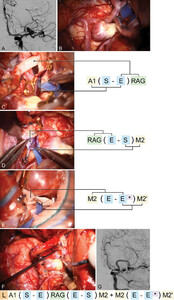
The middle communicating artery (MCoA) was recently introduced as a novel bypass construct between MCA trunks to redistribute flow in the MCA territory in response to changing supply and demand, analogous to the anterior and posterior communicating arteries. The MCoA has been created in three forms with three unique donors: 1) with a double-barrel STA (Fig. 5B), 2) with an interpositional graft from the cervical ECA, and 3) with an interpositional graft from the A1 ACA (Fig. 5C).The codes for these bypasses may appear cumbersome, but the nomenclature conveys details of these sophisticated bypasses that would be lost without it, like the use of the asterisk to denote intraluminal suturing (Fig. 6).

Case example of cerebral bypass coding of the MCoA, which exists only as a bypass construct and does not occur naturally and is constructed using the IC-IC interpositional bypass technique shown inFigure 5C. The intraoperative photographs show the creation of the bypass in a stepwise manner.A:术前血管造影(左ICA血管造影,anteroposterior view) showing the aneurysm located at the MCA bifurcation with the frontal and temporal trunks originating from the base of the aneurysm.B:Intraoperative photograph of the MCA aneurysm in the sylvian fissure.C:Photograph of preparation for the proximal anastomosis in the construction of the MCoA, an A1 (S-E) RAG.D:Intraluminal inspection of the completed first suture line of the distal RAG anastomosis to M2.E:Photograph of the final anastomosis showing end-to-end reimplantation of the frontal and temporal trunks with intraluminal suturing of these two M2 segments.F:Photograph of the completed MCoA bypass with distal clip occlusion of the aneurysm.G:Postoperative angiogram (left ICA angiogram, anterior oblique view) showing the patency of the bypass and the filling of the distal MCA territory. Panels B–F published with permission from Barrow Neurological Institute, Phoenix, AZ.
Ra的三支吻合最近提议vina et al. used a single-donor graft to revascularize two parallel A3 ACAs joined with a half-completed S-S anastomosis.13Two ACAs were sewn together along the deep suture line, and the donor graft was sewn to these half-joined ACAs.13This innovative bypass could be coded as R STA (E-E) RAG (E-S) [L A3 (1/2S-1/2S) R A3].
Discussion
The literature review performed in this study demonstrates the significant ambiguity and imprecision of the existing nomenclature for the reporting of cerebral bypasses in the literature. The current nomenclature is simplistic, prevents a thorough understanding of bypass construction, and omits critical technical details. We propose a new systematic nomenclature that is clear and concise and addresses the current deficiencies of naming bypasses found in the literature. The proposed nomenclature encourages greater precision in describing bypasses, includes technical details that can advance the field, and may improve bypass reporting in the literature. Bypass surgery is remarkably innovative, with novel bypasses appearing regularly in the literature. The adoption of improved and descriptive nomenclature would help capture this dynamic evolution.
There is no substitute for carefully curated intraoperative photographs, videos, and illustrations depicting the stepwise construction of a complex bypass.1,39–42However, these media are not often available, take time to produce, and can be costly. Previously, we introduced a system of symbols (Fig. 2) to diagram bypasses with the intent to improve communication.3,24These symbols are also meant to help bypass surgeons design novel bypasses and hone new bypass concepts. The symbols allow the creation of bypass blueprints before surgery and graphic communication afterward. Although this system of symbols is a valuable teaching tool for compiling cases in a textbook, it has proven to be less applicable as a communication tool or a reporting standard. It is difficult to produce these bypass blueprints for publications or the medical record because there are no commercially available graphic tools for bypasses like those available in architecture, for example. Therefore, written shorthand for bypasses is more likely to have the desired communication impact than symbolic shorthand.
Our proposed nomenclature is simple, succinct, and clear. It is modeled after mathematical formulas, and simple principles like the distributive property can be applied. Critical information is contained within the abbreviated code that can be deciphered and understood by neurosurgeons. Unusual bypass constructs in the literature were easily captured, with high interobserver reliability. In addition, neurosurgeons reading the code have deciphered the constructs with high interobserver reliability. The bypass code includes the essential components of the construct and provides an accurate and precise shorthand description of the bypass for the operative team of assistant surgeons, residents, and nurses. This shorthand can reduce errors, facilitate safe surgery, and improve documentation in the medical record.
拟议的命名法提高了描述of the bypass but does not explicitly describe the surgical approach. The nomenclature captures the segmental anatomy, which is suggestive of the approach. For example, an R STA (E-S) s1 bypass would be approached through an orbitozygomatic transsylvian approach to the oculomotor-tentorial triangle, whereas an R STA (E-S) s2 bypass would be approached through a subtemporal approach to theambient cistern. Statistics on interobserver reliability were not performed because of the limited number of authors. We believe the proposed nomenclature is intuitive, easy to learn, and widely applicable. We introduce it with the hope that other bypass surgeons find value in it, adopt it in their publications and presentations, and ultimately elevate the discourse on bypass surgery.
Conclusions
Bypasses are becoming increasingly complex with the expansion of IC-IC techniques. Descriptions of these constructs with existing nomenclature may be imprecise or confusing, and illustrations and symbolic schematics may not be available. We propose a comprehensive nomenclature based on the segmental anatomy and additional anastomotic details that enables bypasses to be coded simply, succinctly, and accurately. The alphanumeric shorthand encourages greater precision in describing bypasses, improves our reporting in the literature, and includes technical details that could advance the field of bypass surgery.
Acknowledgments
We thank the staff of Neuroscience Publications at Barrow Neurological Institute for assistance with manuscript preparation, illustrations, and graphical application development.
Addendum
Consistent and accurate representation of increasingly complex bypass techniques is a challenge. Ambiguity and lack of a standard nomenclature that captures the nuances of contemporary bypass techniques confound the medical literature and impede the neurosurgical advancement of bypass techniques. We have developed an innovative, standardized bypass coding nomenclature that can code basic to elegantly complex bypasses simply and accurately.
VIDEO 1.Barrow Bypass Coder. This web-based interactive tool allows users to indicate pathologies, build bypasses, and generate the detailed bypass code. Copyright Barrow Neurological Institute, Phoenix, AZ. Published with permission. Clickhereto view.
The desktop computer app is designed for neurosurgeons and neurosurgery residents. It features drag-and-drop symbols for pathologies and treatments and editable blood vessels and grafts to generate the written code. You can find it on the Barrow Neurological Institute website by searching “Barrow Bypass Coder.”
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author Contributions
Conception and design: Lawton, Tayebi Meybodi. Acquisition of data: Tayebi Meybodi, Gadhiya, Borba Moreira. Analysis and interpretation of data: Lawton, Tayebi Meybodi. Drafting the article: Lawton, Tayebi Meybodi. Critically revising the article: Lawton, Tayebi Meybodi. Reviewed submitted version of manuscript: Lawton, Tayebi Meybodi. Statistical analysis: Lawton, Tayebi Meybodi. Administrative/technical/material support: Lawton, Tayebi Meybodi. Study supervision: Lawton.
Supplemental Information
Videos
Video 1.https://vimeo.com/533464120.
References
-
1 ↑
WesselsL,FekonjaLS,VajkoczyP.Bypass surgery of complex middle cerebral artery aneurysms—technical aspects and outcomes.Acta Neurochir (Wien).2019;161(10):1981–1991.
-
2
NatarajanSK,ZeeshanQ,GhodkeBV,SekharLN.Brain bypass surgery for complex middle cerebral artery aneurysms: evolving techniques, results, and lessons learned.World Neurosurg.2019;130:e272–e293.
-
3 ↑
Tayebi MeybodiA,HuangW,BenetA,et al.Bypass surgery for complex middle cerebral artery aneurysms: an algorithmic approach to revascularization.J Neurosurg.2017;127(3):463–479.
-
4
SanaiN,ZadorZ,LawtonMT.Bypass surgery for complex brain aneurysms: an assessment of intracranial-intracranial bypass.开云体育app官方网站下载入口.2009;65(4):670–683.
-
5
BaranoskiJF,PrzybylowskiCJ,MascitelliJR,et al.Anterior inferior cerebellar artery bypasses: the 7-bypass framework applied to ischemia and aneurysms in the cerebellopontine angle.Oper Neurosurg (Hagerstown).2020;19(2):165–174.
-
6
Tayebi MeybodiA,BenetA,LawtonMT.The V3 segment of the vertebral artery as a robust donor for intracranial-to-intracranial interpositional bypasses: technique and application in 5 patients.J Neurosurg.2018;129(3):691–701.
-
7
RubioRR,GandhiS,VigoV,et al.an anatomic feasibility study for revascularization of the ophthalmic artery, part I: intracanalicular segment.World Neurosurg.2020;133:e893–e901.
-
8
Tayebi MeybodiA,LawtonMT,GriswoldD,et al.Revascularization of the upper posterior circulation with the anterior temporal artery: an anatomical feasibility study.J Neurosurg.2018;129(1):121–127.
-
9 ↑
RussinJJ.The arborization bypass: sequential intracranial-intracranial bypasses for an unruptured fusiform MCA aneurysm.J Clin Neurosci.2017;39:209–211.
-
10
KatoN,PrinzV,FingerT,et al.Multiple reimplantation technique for treatment of complex giant aneurysms of the middle cerebral artery: technical note.Acta Neurochir (Wien).2013;155(2):261–269.
-
11 ↑
MirzadehZ,SanaiN,LawtonMT.The azygos anterior cerebral artery bypass: double reimplantation technique for giant anterior communicating artery aneurysms.J Neurosurg.2011;114(4):1154–1158.
-
12
LeeSH,ChoiSK.In situ intersegmental anastomosis within a single artery for treatment of an aneurysm at the posterior inferior cerebellar artery: closing omega bypass.J Korean Neurosurg Soc.2015;58(5):467–470.
-
13 ↑
RavinaK,YimB,LamJ,et al.Three-vessel anastomosis for direct bihemispheric cerebral revascularization.Oper Neurosurg (Hagerstown).2020;19(3):313–318.
-
14
BenetA,MontemurroN,LawtonMT.Management of a ruptured posterior inferior cerebellar artery (PICA) aneurysm with PICA-PICA in situ bypass and trapping: 3-dimensional operative video.Oper Neurosurg (Hagerstown).2017;13(3):400.
-
15
MeybodiAT,LawtonMT,BenetA.Sequential extradural release of the V3 vertebral artery to facilitate intradural V4 vertebral artery reanastomosis: feasibility of a novel revascularization technique.Oper Neurosurg (Hagerstown).2017;13(3):345–351.
-
16
LawtonMT,AblaAA,RutledgeWC,et al.Bypass surgery for the treatment of dolichoectatic basilar trunk aneurysms: a work in progress.开云体育app官方网站下载入口.2016;79(1):83–99.
-
17
AblaAA,LawtonMT.Revascularization for unclippable posterior inferior cerebellar artery aneurysms: extracranial-intracranial or intracranial-intracranial bypass?World Neurosurg.2014;82(5):586–588.
-
18
Tayebi MeybodiA,LawtonMT,GriswoldD,et al.The anterior temporal artery: an underutilized but robust donor for revascularization of the distal middle cerebral artery.J Neurosurg.2017;127(4):740–747.
-
19
KalaniMY,RameyW,AlbuquerqueFC,et al.Revascularization and aneurysm surgery: techniques, indications, and outcomes in the endovascular era.开云体育app官方网站下载入口.2014;74(5):482–498.
-
20
AblaAA,LawtonMT.The superficial temporal artery trunk-to-M2 middle cerebral artery bypass with short radial artery interposition graft: the forgotten bypass.World Neurosurg.2015;83(2):145–146.
-
21 ↑
AblaAA,LawtonMT.Anterior cerebral artery bypass for complex aneurysms: an experience with intracranial-intracranial reconstruction and review of bypass options.J Neurosurg.2014;120(6):1364–1377.
-
22
Tayebi MeybodiA,LawtonMT,GriswoldD,et al.Assessment of the temporopolar artery as a donor artery for intracranial-intracranial bypass to the middle cerebral artery: anatomic feasibility study.World Neurosurg.2017;104:171–179.
-
23
MuraJ,RiquelmeF,CuevasJL,et al.简化的单一器官前大脑旁路:y-shaped superficial temporal artery interposition graft from A2 with double reimplantation of pericallosal arteries: technical case report.开云体育app官方网站下载入口.2013;72(2 Suppl Operative):onsE235–ons240.
-
26 ↑
Rodríguez-HernándezA,RhotonALJr,LawtonMT.Segmental anatomy of cerebellar arteries: a proposed nomenclature. Laboratory investigation.J Neurosurg.2011;115(2):387–397.
-
27 ↑
LawtonMT,LangMJ.The future of open vascular neurosurgery: perspectives on cavernous malformations, AVMs, and bypasses for complex aneurysms.J Neurosurg.2019;130(5):1409–1425.
-
28
DuckworthEA,饶VY,PatelAJ.Double-barrel bypass for cerebral ischemia: technique, rationale, and preliminary experience with 10 consecutive cases.开云体育app官方网站下载入口.2013;73(1 Suppl Operative):ons30-8–ons37-8.
-
29
NakajimaH,KamiyamaH,NakamuraT,et al.直接手术治疗巨大颅内eurysms on the anterior communicating artery or anterior cerebral artery.Neurol Med Chir (Tokyo).2013;53(3):153–156.
-
30
CantoreG,SantoroA,GuidettiG,et al.Surgical treatment of giant intracranial aneurysms: current viewpoint.开云体育app官方网站下载入口.2008;63(4)(suppl 2):279–290.
-
31
HongoK,HoriuchiT,NittaJ,et al.Double-insurance bypass for internal carotid artery aneurysm surgery.开云体育app官方网站下载入口.2003;52(3):597–602.
-
32
OtaniN,WadaK,SakakibaraF,et al.“Reverse” bypass using a naturally formed “bonnet” superficial temporal artery in symptomatic common carotid artery occlusion: a case report.Neurol Med Chir (Tokyo).2014;54(10):851–853.
-
33
BulsaraKR,PatelT,FukushimaT.Cerebral bypass surgery for skull base lesions: technical notes incorporating lessons learned over two decades.Neurosurg Focus.2008;24(2):E11.
-
34
WadaK,OtaniN,ToyookaT,et al.Superficial temporal artery to anterior cerebral artery hemi-bonnet bypass using radial artery graft for prevention of complications after surgical treatment of partially thrombosed large/giant anterior cerebral artery aneurysm.J Stroke Cerebrovasc Dis.2018;27(12):3505–3510.
-
35 ↑
EndoH,SugiyamaSI,EndoT,et al.Revascularization of the anterior cerebral artery by Y-shaped superficial temporal artery interposition graft for the treatment of a de novo aneurysm arising at the site of A3-A3 bypass: technical case report.J Neurosurg.2018;129(5):1120–1124.
-
36 ↑
DenglerJ,KatoN,VajkoczyP.The Y-shaped double-barrel bypass in the treatment of large and giant anterior communicating artery aneurysms.J Neurosurg.2013;118(2):444–450.
-
37 ↑
SpetzlerRF,RoskiRA,RhodesRS,ModicMT.The “bonnet bypass.”. Case report.J Neurosurg.1980;53(5):707–709.
-
38 ↑
LawtonMT,Quiñones-HinojosaA.Double reimplantation technique to reconstruct arterial bifurcations with giant aneurysms.开云体育app官方网站下载入口.2006;58(4)(suppl 2):ONS-347–ONS-354.
-
39
BurkhardtJK,YousefS,TabaniH,et al.Combination superficial temporal artery-middle cerebral artery bypass and M2-M2 reanastomosis with trapping of a stented distal middle cerebral artery aneurysm: 3-dimensional operative video.Oper Neurosurg (Hagerstown).2018;15(5):E67–E68.
-
40
GandhiS,RodriguezRL,TabaniH,et al.Double-barrel extracranial-intracranial bypass and trapping of dolichoectatic middle cerebral artery aneurysms: 3-dimensional operative video.Oper Neurosurg (Hagerstown).2019;17(1):E14–E15.
-
41
OtaN,PetrakakisI,KondoT,et al.Complex bypass surgery for multiple fusiform aneurysms, including a thrombosed giant aneurysm of the middle cerebral artery.World Neurosurg.2020;138:284.
-
42
ParkDH,SinghH,da SilvaHB,SekharLN.Side-to-side A3-A4 bypass after clip ligation of recurrent coiled anterior communicating artery aneurysm: 3-dimensional operative video.Oper Neurosurg (Hagerstown).2018;14(1):87.